Table of Contents
Credits
Host: Sara Dong
Guests: Jonathan Ryder, Sarah Turbett
Writing: Sara Dong
Edited and produced by Sara Dong with support from the Infectious Diseases Society of America (IDSA)
Our Guests
Jonathan Ryder, MD

Dr. Ryder is an assistant professor in the Division of Infectious Diseases at the University of Nebraska Medical Center. He serves as the associate medical director of antimicrobial stewardship and associate hospital epidemiologist in the infection control and epidemiology program. He has academic interests in diagnostic stewardship, stewardship in rural settings, and digital medical education.
Sarah Turbett, MD

Dr. Turbett is an Assistant Professor of Medicine in the Division of Infectious Diseases and Department of Pathology at the Massachusetts General Hospital. She received her medical degree from the Albert Einstein College of Medicine and completed her training in infectious diseases at the combined program for infectious diseases at the Massachusetts General Hospital and Brigham and Women’s Hospital with a focus on transplant infectious diseases and care of the immunocompromised host. She has also completed a fellowship in clinical microbiology at the Massachusetts General Hospital and serves as an Associate Laboratory Director for the Microbiology laboratory at MGH. Areas of interest include clinical lab test utilization and stewardship, antimicrobial resistance, and emerging infectious diseases.
Culture
Jonathan has been watching Rings of Power season 2
Sarah enjoys some Bravo reality TV and Love Island as an escape
Consult Notes
Consult Q
Should I get blood cultures?
Key Points
We discussed briefly the BD BACTEC blood culture bottle shortage. Here is a quick overview and some of the mentioned resources
- This summer in June, labs/hospitals were notified about how BD Diagnostics was experiencing reduced availability of plastic blood culture bottles from their supplier – and the expectation for temporary shortage of BD BACTEC aerobic, anaerobic, pediatric, and fungal/mycobacterial blood culture bottles in the US as well as globally
- Among several mitigation steps was moving to temporary sourcing of glass vials for 1 type of media (BD BACTEC™ Lytic/10 Anaerobic/F Culture Vials)
- FDA Letter from July 10, 2024 – https://www.fda.gov/medical-devices/letters-health-care-providers/disruptions-availability-bd-bactec-blood-culture-media-bottles-letter-health-care-providers
- CDC/IDSA Clinician Call: BD BACTEC Blood Culture Bottle Shortage (jointly hosted with ASM, SHEA, PIDS)
- IDSA Blood Culture Bottle Shortage Page with various resources
- BD BACTEC Blood Culture Supply Update Page
- American Society for Microbiology Managing Blood Culture Bottle Shortage page
- Preventing adult blood culture contamination: a quality tool for clinical laboratory professionals
- SHEA: Principles of diagnostic stewardship – A practical guide
Key take-homes to remember related to blood culture collection
- Drawing blood cultures only when indicated (preventing “rainbow draws”)
- Avoiding blood culture contamination to help us with both antibiotic and blood culture overuse. This includes:
- Avoid drawing blood through indwelling intravenous or intra-arterial catheters unless blood cannot be obtained by venipuncture or the diagnosis of catheter-related infection is suspected. Blood cultures obtained from venous access devices such as IV catheters and ports are associated with greater contamination rates than blood cultures obtained by venipuncture.
- Hand hygeine
- Proper cleansing of venipuncture site: appropriate disinfectants, double cleanse methods (alcohol and let dry followed by second disinfected. Avoid touching venipuncture area after it has been cleaned unless wearing sterile gloves
- If high contamination rates, can consider discard tube or discard devices
- Each hospital should know their contamination rates. Goal <3% but ideally <1% (CLSI benchmark). Accrediting agencies require contamination rate monitoring.
- Ensure proper volume of blood collected
- Volume of blood collected for each blood culture is most critical variable in recovering bacteria and fungi from patients with bloodstream infections.
- Too little blood – lower sensitivity for detection
- Too much blood – higher risk of contaminants and false positives
- Not timing!
- It used to be thought that blood cultures had to be separated in time. Now just separated in terms of site of collection, can be drawn at the same time/simultaneously.
- Fabre V, Jones GF, Hsu YJ, Carroll KC, Cosgrove SE; CDC Prevention Epicenters Program. To wait or not to wait: Optimal time interval between the first and second blood-culture sets to maximize blood-culture yield. Antimicrob Steward Healthc Epidemiol. 2022;2(1):e51. Published 2022 Mar 25. doi:10.1017/ash.2022.27.
- You do want them before antibiotic administration though!
- It used to be thought that blood cultures had to be separated in time. Now just separated in terms of site of collection, can be drawn at the same time/simultaneously.
- Volume of blood collected for each blood culture is most critical variable in recovering bacteria and fungi from patients with bloodstream infections.
- For adults, 20-30 mL of blood per culture set is recommended and may require inoculation of 2 culture bottles depending on system. Both aerobic and anaerobic bottles should be inoculated. Aerobic bottle always inoculated first as tend to cultivate more organisms with this bottle.
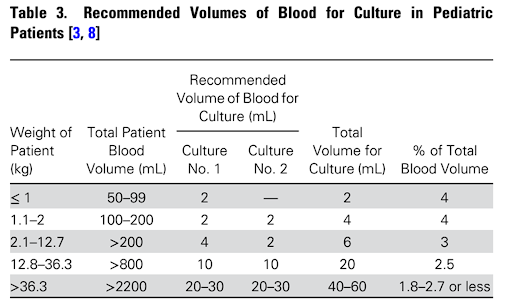
- For children, an age- and weight- appropriate volume of blood should be cultured. Use 1-2 aerobic bottles for children. Anaerobic bottles added if concern for anaerobic infection (intra-abdominal pathology for example)
- Number of blood culture sets:
- Ideally at least 2 as:
- 8-12% of bacteremias are picked up with a second set
- Helps determine true BSI vs. contaminant for certain organisms (commensals)
- Degree of bacteremia can be informative (high grade vs. low grade)
- Blood culture bottle transport: get to the lab as soon as possible, ideally within 4 hrs
Blood culture stewardship references
- Jonathan gave an overview of stewardship of blood culture indications. You can check out this paper as well: Ryder JH, Van Schooneveld TC, Diekema DJ, Fabre V. Every Crisis Is an Opportunity: Advancing Blood Culture Stewardship During a Blood Culture Bottle Shortage. Open Forum Infect Dis. 2024;11(9):ofae479. Published 2024 Aug 23. doi:10.1093/ofid/ofae479
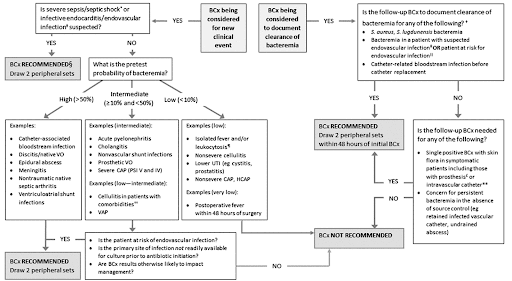
- Scoping review and algorithm mentioned on use of blood cultures in common clinical scenarios: Fabre V, Sharara SL, Salinas AB, Carroll KC, Desai S, Cosgrove SE. Does This Patient Need Blood Cultures? A Scoping Review of Indications for Blood Cultures in Adult Nonneutropenic Inpatients. Clin Infect Dis. 2020 Aug 22;71(5):1339-1347. doi: 10.1093/cid/ciaa039. PMID: 31942949.
- This paper helped to calculate the pre-test probability of bacteremia, and these were divided into high probability (>50%), intermediate probability (10-50%), and low probability (<10%)
- An algorithm along with clinician education were implemented int he DISTRIBUTE study in adult ICUs and medical wards, which reduced blood culture utilization, increased rate of recovery of true pathogens, and decreased single blood culture use: Fabre V, Klein E, Salinas AB, Jones G, Carroll KC, Milstone AM, Amoah J, Hsu YJ, Gadala A, Desai S, Goyal A, Furfaro D, Zimmerman J, Lin S, Cosgrove SE. A Diagnostic Stewardship Intervention To Improve Blood Culture Use among Adult Nonneutropenic Inpatients: the DISTRIBUTE Study. J Clin Microbiol. 2020 Sep 22;58(10):e01053-20. doi: 10.1128/JCM.01053-20. PMID: 32759354; PMCID: PMC7512168.
- You can also check out this resource: JHU Blood Culture Stewardship
- http://HopkinsChildrens.org/brightstar
- https://www.hopkinsmedicine.org/antimicrobial-stewardship
- In Jan 2014, a multidisciplinary team at Johns Hopkins Children’s Center developed and implemented a clinical practice strategy to guide clinicians in the use of blood cultures when evaluating pts with signs/sxs of sepsis
- All of these hospitals had local QI programs to improve blood cx use in the ICU → and they found:
- 33% relative reduction in bcx rate
- 36% relative reduction in CLABSI rate
- 13% relative reduction in broad-spectrum antibiotic use
- Safe: no difference in mortality, PICU readmission, PICU LOS before and after the intervention, number of sepsis, severe sepsis/septic shock cases before and after the intervention
- Woods-Hill CZ, Colantuoni EA, Koontz DW, Voskertchian A, Xie A, Thurm C, Miller MR, Fackler JC, Milstone AM; Bright STAR Authorship Group; Agulnik A, Albert JE, Auth MJ, Bradley E, Clayton JA, Coffin SE, Dallefeld S, Ezetendu CP, Fainberg NA, Flaherty BF, Foster CB, Hauger SB, Hong SJ, Hysmith ND, Kirby AL, Kociolek LK, Larsen GY, Lin JC, Linam WM, Newland JG, Nolt D, Priebe GP, Sandora TJ, Schwenk HT, Smith CM, Steffen KM, Tadphale SD, Toltzis P, Wolf J, Zerr DM. Association of Diagnostic Stewardship for Blood Cultures in Critically Ill Children With Culture Rates, Antibiotic Use, and Patient Outcomes: Results of the Bright STAR Collaborative. JAMA Pediatr. 2022 Jul 1;176(7):690-698. doi: 10.1001/jamapediatrics.2022.1024. PMID: 35499841; PMCID: PMC9062771.
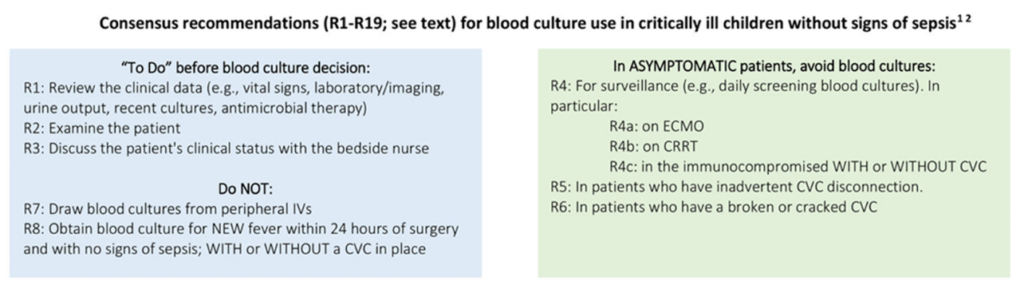
- You can also find the Bright Star consensus recommendations for blood culture use in critically ill children:
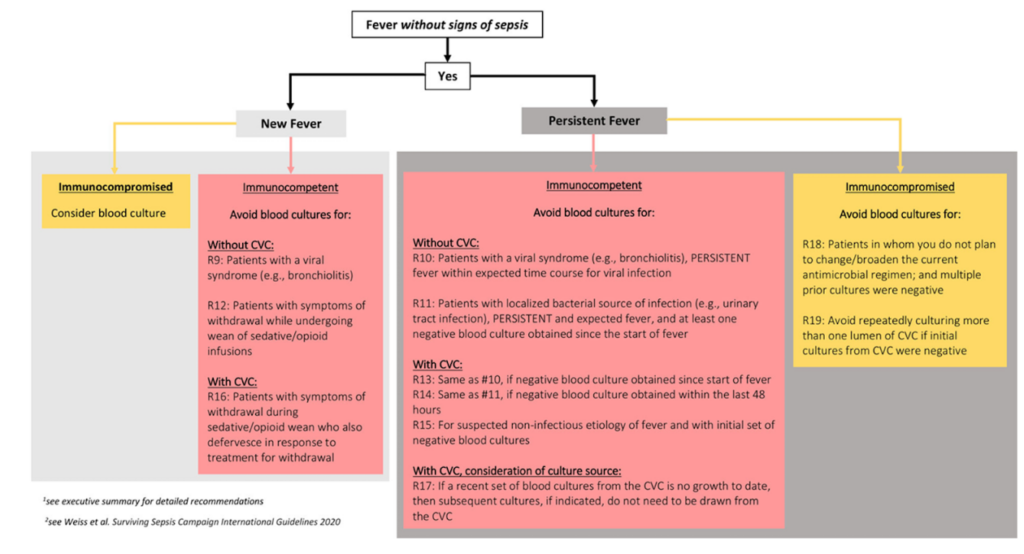
- They have a similar algorithm that has guidance on general recommendations as well as looking at blood culture practices in symptomatic immunocompetent vs immunocompromised children
- Woods-Hill CZ, Koontz DW, Voskertchian A, Xie A, Shea J, Miller MR, Fackler JC, Milstone AM; Bright Star Consensus Authorship Group. Consensus Recommendations for Blood Culture Use in Critically Ill Children Using a Modified Delphi Approach. Pediatr Crit Care Med. 2021 Sep 1;22(9):774-784. doi: 10.1097/PCC.0000000000002749. PMID: 33899804; PMCID: PMC8416691.
We also spoke about work from the Bright Star Consensus Group in pediatrics:
Infographics
Goal
Listeners will be able to understand blood culture stewardship
Learning Objectives
After listening to this episode, listeners will be able to:
- Discuss available literature related to pre-test probability of infections that may cause bloodstream infection
- List strategies to ensure proper blood culture collection
- Identify features of an action plan that could be used during a shortage
Disclosures
Febrile podcast and hosts report no relevant financial disclosures
Jonathan Ryder disclosure: Receives funding from the Johns Hopkins Prevention Epicenter Blood Culture Stewardship Collaborative funded by CDC’s Prevention Epicenters Program. The content in the podcast is solely the responsibility of the authors and does not represent the official view of the funding agency.
Sarah Turbett disclosure: Consultant for CARB-X. Receives funding from SeLux Diagnostics
Citation
Turbett, S., Ryder, J., Dong, S. “#112: When to draw blood cultures”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/2071920a-1b11-44da-a74f-58a89af4293f/