Table of Contents
Credits
Host: Sara Dong
Guests: Tom Schmidt, George R Thompson, Nate Bahr
Written, Edited and Produced by Sara Dong with support from the Infectious Diseases Society of America (IDSA)
Our Guests
Tom Schmidt, MD, MHS

Tom Schmidt, MD, MHS is a second year adult infectious diseases fellow at the University of Minnesota. He is interested in general ID, critical care, and the impact of a changing climate on infectious diseases.
George R. Thompson III, MD

George R. Thompson III, M.D., is a professor of Medicine at the University of California, Davis, School of Medicine with a joint appointment in the Departments of Medical Microbiology and Immunology, and Internal Medicine, Division of Infectious Diseases. Dr. Thompson specializes in the care of patients with invasive fungal infections and has research interests are in fungal diagnostics, clinical trials, novel antifungal agents, and host immunogenetics. Dr. Thompson has served on the IDSA Journal Club is a member of the Coccidioidomycosis Study Group Executive Committee, and is president-elect of the Mycoses Study Group.
Nate Bahr, MD, FIDSA

Nate Bahr, MD, FIDSA is an associate professor in the Division of Infectious Diseases at the University of Minnesota. His areas of interest include histoplasmosis, the changing epidemiology of fungal infections, drug pricing, cryptococcal meningitis and TB meningitis. Dr. Bahr is a co-chair of the education committee of the Mycoses Study Group Education and Research Consortium, along with Dr. Jessica Little
Culture
Tom: birdwatching (his favorites are the white breast, nut hatch, golden eagle)
GR: keeping up with his children at their various sports/activities like lacrosse and golf
Nate: loves spending time with his kids and enjoyed playing in the snow with them this winter
Consult Notes
Consult Q
50 yo man who presents with two weeks of fatigue, fevers, chills, and a new cough despite outpatient bacterial pneumonia treatment
Case Summary
50 yo man with hypertension and diabetes mellitus type 2 who was found to have primary pulmonary coccidioidomycosis
Key Points
Learn more and join MSGERC!
- The Mycoses Study Group Education & Research Consortium is dedicated to championing the diagnosis, prevention, treatment, and management of invasive fungal infections.
- Check out the webpage: https://msgerc.org/
- In particular, check out their Education resources here: https://msgerc.org/education-resources/
- Follow MSGERC on Bluesky: https://bsky.app/profile/msgerc.bsky.social
- Here is the recent webinar we mentioned: Coccidioidomycosis: Clinical considerations in the aftermath of wildfires

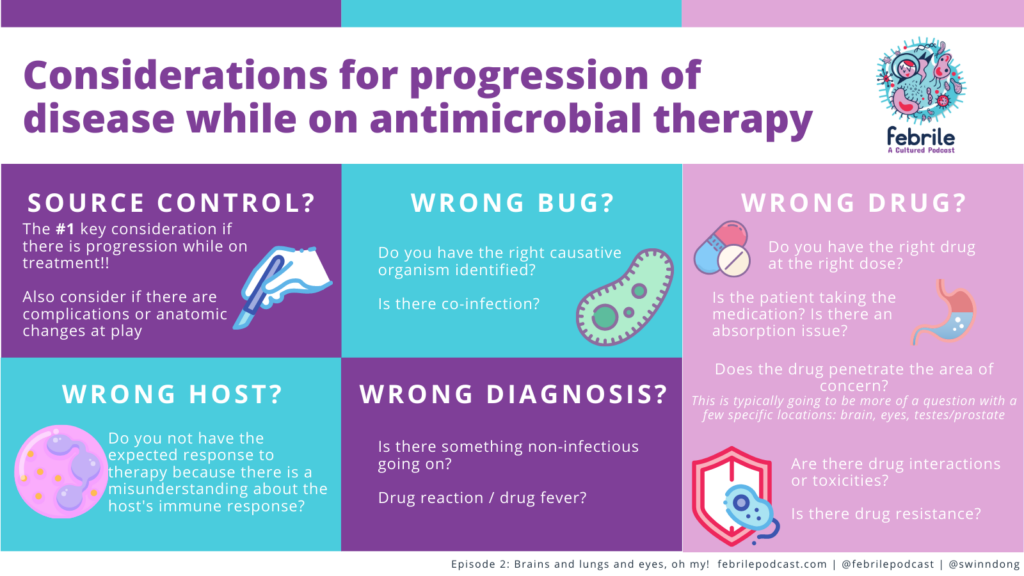
We discussed considerations for when patients have progression of disease despite antimicrobials. Here is an older Febrile graphic on this!
The expanding maps for endemic mycoses: Don’t rule out an endemic mycoses just because of your geographic area! As Nate explained, this is just one factor in the calculus
- We discussed the growing literature related to the expanding presence of endemic fungi
- Here is the paper we directly mentioned that uses published literature to update the endemic fungi maps: Ashraf N, Kubat RC, Poplin V, et al. Re-drawing the Maps for Endemic Mycoses. Mycopathologia. 2020;185(5):843-865. doi:10.1007/s11046-020-00431-2
- Another recent paper on the geographic distribution of dimorphic mycoses: Mazi PB, Sahrmann JM, Olsen MA, et al. The Geographic Distribution of Dimorphic Mycoses in the United States for the Modern Era. Clin Infect Dis. 2023;76(7):1295-1301. doi:10.1093/cid/ciac882
- A paper from those who found evidence of Histoplasma in soil and penguin excreta in Antartica: Moreira LM, Meyer W, Chame M, et al. Molecular Detection of Histoplasma capsulatum in Antarctica. Emerg Infect Dis. 2022;28(10):2100-2104. doi:10.3201/eid2810.220046
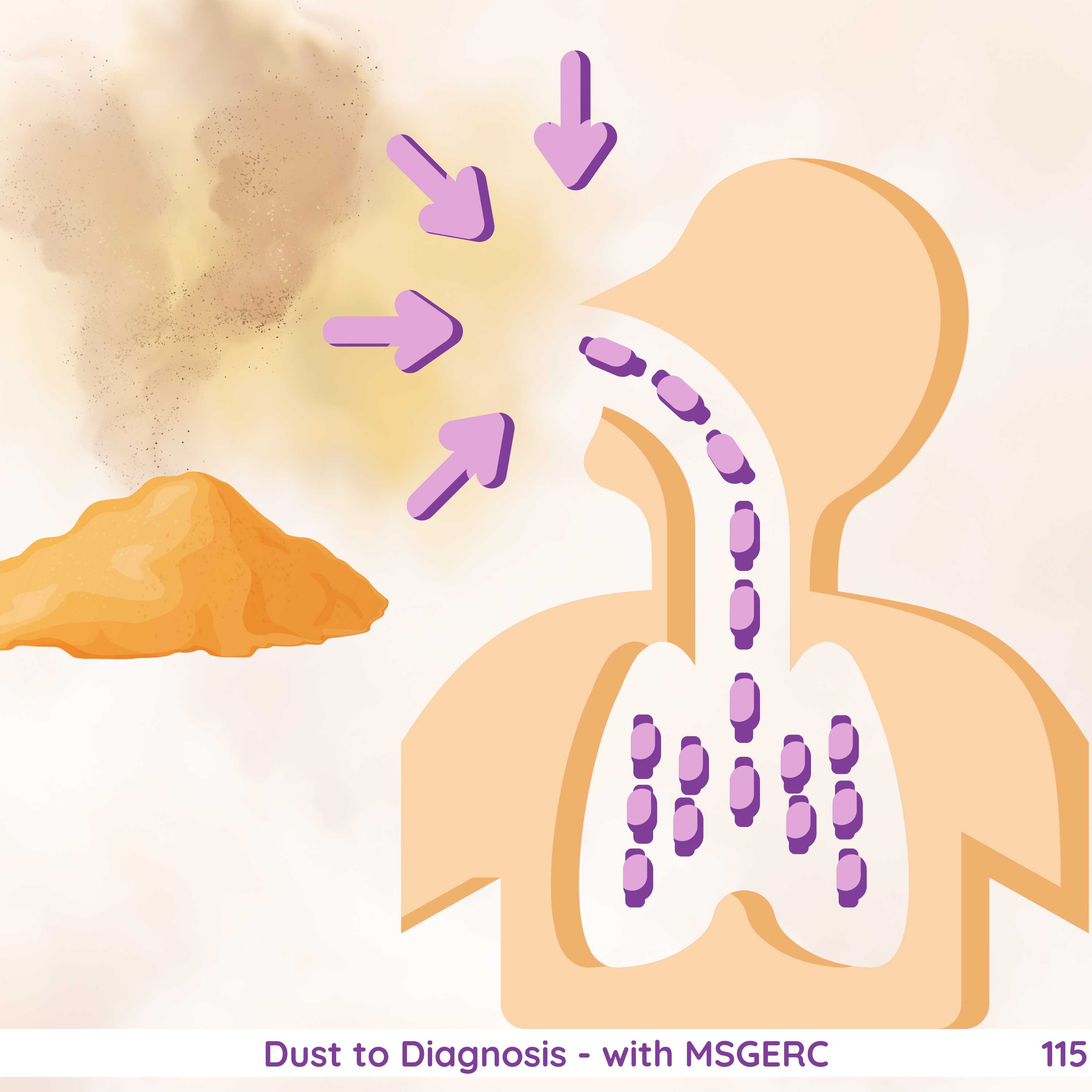
A quick intro to the focus of this episode: coccidioidomycosis!
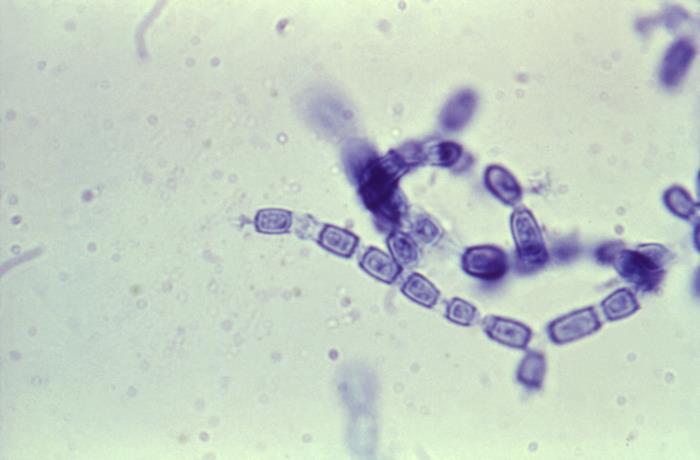
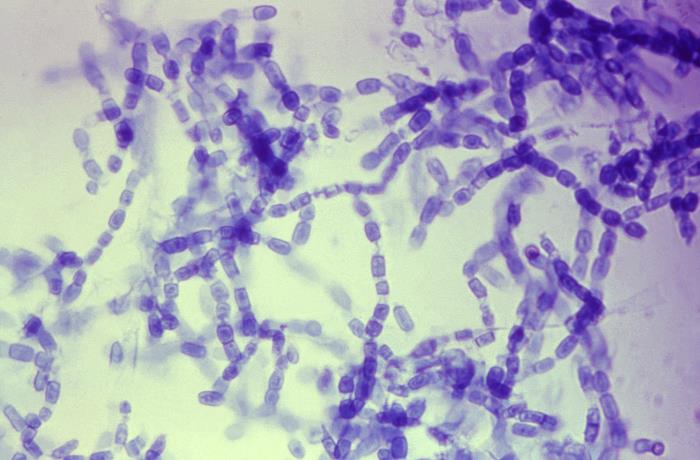
- Coccidioidomycosis: caused by the dimorphic fungi Coccidioides
- The two species: C.immitis, C.posadasii (there’s no major clinical difference between the species, labs don’t routinely distinguish between them)
- The acute pneumonia is sometimes called Valley fever, but there is a wide range of clinical illnesses that can result for Cocci infection
- Coccidioides grows as a mold close to the surface of soil
- The mycelia produce spore-bearing branches that grow upward into the air —> alternating cells degenerate and release single cells called arthroconidia
- The arthroconidia can remain suspended for prolonged times in the air —> then can penetrate airways when inhaled —> the barrel-shaped arthroconidia enalrge to become spherules in the lung —> eventually enlarging to produce septations
- Cocci is endemic to Western Hemisphere in areas of the US, northern Mexico, and areas of Central and South America
- In the US, most cases of cocci are reported from the San Joaquin Valley of California or from south-central region of Arizona (including Maricopa and Pima counties; Phoenix; Tucson) —> but of course other regions have reported cases as well like other areas in southern CA, southern NV, southwest UT, and southern NM
- The risk of exposure is typically seasonal and highest in dry periods/droughts following a rainy season
Coccidioides clinical presentation
- Coccidioidomycosis can have asymptomatic infection
- This episode focused on primary pulmonary infection / pneumonia. A few key points:
- Incubation period ranges between 7-21 days after an exposure
- Various clinical presentations may occur such as localized pneumonia or diffuse pulmonary disease. Systemic symptoms, rheumatologic complaints, and skin findings may be present as well
- As GR discussed, this could appear just like a bacterial CAP and in endemic areas, up to ~29% of CAP cases are cocci
- This episode also mentioned the possibility of cutaneous manifestations like erythema nodosum (painful, erythematous nodules on lower extremities). Tip from GR: development of erythema nodosum is a favorable prognostic sign—> it’s not disseminated infection, it’s a sign that you’re starting to develop Th1 immunity to the underlying Cocci spp
- Peripheral blood eosinophilia can be seen in about a quarter of patients
- There are also extrapulmonary manifestations of cocci! The episode briefly touched on CNS disease, which can occur in some patients.
- GR discussed how even uncomplicated pulmonary infection can be accompanied by headache
- Headache characteristics that would be more suggestive of meningitis in a patient with coccidioidal pneumonia:
- Persistent headache
- Progressive worsening of headache
- Unusual severity of headache
- Associated nausea/vomiting
- Blurry vision
- Mental status changes
- The threshold for LP would also be lower in those who are immunocompromised
- Here is an article on changing the dogma, that routine LP is not unnecessary if patient’s don’t have CNS symptoms: Thompson G 3rd, Wang S, Bercovitch R, et al. Routine CSF analysis in coccidioidomycosis is not required. PLoS One. 2013;8(5):e64249. Published 2013 May 22. doi:10.1371/journal.pone.0064249
Risk factors for severe and disseminated coccidioidomycosis
GR discussed some groups that are at increased risk for severe or disseminated disease including:
- Older patients ≥65 years old
- Patients with diabetes mellitus
- Those with underlying defects in cellular immunity (such as transplantation, HIV with CD4 <250, and others)
- Ancestral genomic background: studies have noted high rates of cocci in those with African or Filipino ancestry. GR mentioned some work from Drs. Amy Hsu and Steven Holland, here are a few resources on genetic determinates and severity of cocci:
- Galgiani JN, Hsu AP, Powell DA, Vyas JM, Holland SM. Genetic and Other Determinants for the Severity of Coccidioidomycosis: A Clinician’s Perspective. J Fungi (Basel). 2023;9(5):554. Published 2023 May 11. doi:10.3390/jof9050554
- Hsu AP, Korzeniowska A, Aguilar CC, et al. Immunogenetics associated with severe coccidioidomycosis. JCI Insight. 2022;7(22):e159491. Published 2022 Nov 22. doi:10.1172/jci.insight.159491
- Hung CY, Hsu AP, Holland SM, Fierer J. A review of innate and adaptive immunity to coccidioidomycosis. Med Mycol. 2019;57(Supplement_1):S85-S92. doi:10.1093/mmy/myy146
- Infection during pregnancy
Coccidioides diagnostics
- GR explained that the testing for Cocci may be mostly based on workflow at your particular institution, but in most cases:
- Serologic tests using EIA for IgM and IgG are typically ordered first as screening test
- If either or both of IgM and IgG are positive, then followed by immunodiffusion and complement fixation testing
- Serial CF testing provides diagnostic and prognostic information
- Although no precise titer can predict, most clinicians become concerned with titers ≥1:32 (about half of those patients with high titers will have disseminated infection)
- There can be major differences based on which lab runs the titers —> so can’t compare CF titer lab to lab, make sure they are from same lab location!
- Here is the recent CDC publication on algorithms for endemic fungi diagnostics: Smith DJ, Free RJ, Thompson GR 3rd, et al. Clinical Testing Guidance for Coccidioidomycosis, Histoplasmosis, and Blastomycosis in Patients With Community-Acquired Pneumonia for Primary and Urgent Care Providers. Clin Infect Dis. 2024;78(6):1559-1563. doi:10.1093/cid/ciad619
General approach to treatment of coccidioidal pneumonia
- As GR explained, it’s important to consider the severity of illness and patient’s risk factors when considering treatment
- In general, antifungal therapy is not necessary for healthy immunocompetent patients with mild symptoms (no evidence of extensive disease or major risk factors)
- For more moderate or severe diseases or those with risk factors/immunocompromised, treatment is azole therapy. GR talked through some of those options:
- Fluconazole is typical initial therapy
- If patient doesn’t respond or has issues with fluconazole side effects (such as alopecia, cheilitis, xerosis), alternatives include below (which actually have better in vitro activity)
- Itraconazole
- Posaconazole
- Voriconazole
- Isavuconazole
- Here is the one comparative study looking at fluconazole vs itraconazole: Galgiani JN, Catanzaro A, Cloud GA, et al. Comparison of oral fluconazole and itraconazole for progressive, nonmeningeal coccidioidomycosis. A randomized, double-blind trial. Mycoses Study Group. Ann Intern Med. 2000;133(9):676-686. doi:10.7326/0003-4819-133-9-200011070-00009
- With severe or complicated disease, can reach for amphotericin B
- GR discussed how it is a fairly small group that wouldn’t respond to a second triazole and commented on briefly clinical resistance. In addition, he pointed out how we could lose susceptibility to antifungal drugs if their presence on agricultural crops are ignored (for example ipflufenoquin actually works just like olorofim and aminopyrifen works just like fosmanogepix, which we could lose if those are put down in high concentrations in the environment
Climate change and infectious diseases
- We touched on the importance of climate change and major weather events on infectious diseases, including cocci and wildfires
- Here are some papers related to pyroaerobiology!
- Kobziar LN, Thompson GR 3rd. Wildfire smoke, a potential infectious agent. Science. 2020;370(6523):1408-1410. doi:10.1126/science.abe8116
- Kobziar LN, Lampman P, Tohidi A, et al. Bacterial Emission Factors: A Foundation for the Terrestrial-Atmospheric Modeling of Bacteria Aerosolized by Wildland Fires. Environ Sci Technol. 2024;58(5):2413-2422. doi:10.1021/acs.est.3c05142
- Ellington AJ, Walters K, Christner BC, et al. Dispersal of microbes from grassland fire smoke to soils [published correction appears in ISME J. 2024 Jan 8;18(1):wrae232. doi: 10.1093/ismejo/wrae232.]. ISME J. 2024;18(1):wrae203. doi:10.1093/ismejo/wrae203
- Kobziar LN, Vuono D, Moore R, et al. Wildland fire smoke alters the composition, diversity, and potential atmospheric function of microbial life in the aerobiome. ISME Commun. 2022;2(1):8. Published 2022 Jan 25. doi:10.1038/s43705-022-00089-5
- These authors identified an increase in cocci infections after exposure to wildfires: Mulliken JS, Hampshire KN, Rappold AG, Fung M, Babik JM, Doernberg SB. Risk of systemic fungal infections after exposure to wildfires: a population-based, retrospective study in California. Lancet Planet Health. 2023;7(5):e381-e386. doi:10.1016/S2542-5196(23)00046-3
- Here is a paper on a cocci outbreak among inmate wildland firefighters: Laws RL, Jain S, Cooksey GS, et al. Coccidioidomycosis outbreak among inmate wildland firefighters: California, 2017. Am J Ind Med. 2021;64(4):266-273. doi:10.1002/ajim.23218
- Pearson D, Ebisu K, Wu X, Basu R. A Review of Coccidioidomycosis in California: Exploring the Intersection of Land Use, Population Movement, and Climate Change. Epidemiol Rev. 2019;41(1):145-157. doi:10.1093/epirev/mxz004
- Here is a current preprint on detection of airborne cocci: Radosevich MT, Dobson S, Weaver AK, et al. Detection of airborne Coccidioides spores using lightweight portable air samplers affixed to uncrewed aircraft systems in California’s Central Valley. Preprint. bioRxiv. 2025;2024.10.28.620741. Published 2025 Jan 6. doi:10.1101/2024.10.28.620741
Infographics
Goal
Listeners will be able to discuss the diagnosis and clinical features of coccidiomycosis
Learning Objectives
After listening to this episode, listeners will be able to:
- Construct a differential diagnosis of a pneumonia that is not responding to typical antibiotics
- Discuss diagnostic testing for Coccidioides and Blastomyces
- Compare and contrast available antifungal with activity against Cocci
- Define pyroaerobiology
Disclosures
Our guests as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Schmidt, T., Thompson, GR., Bahr, N., Dong, S. “#115: Dust to Diagnosis – with MSGERC”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/a3e69be3-8224-44b2-ad7c-2e93dd251e73/