Table of Contents
Credits
Host(s): Nathan Nolan, Sara Dong
Guest: Raagini Jawa
Writing: Nathan Nolan, Sara Dong
Producing/Editing/Cover Art/Infographics: Sara Dong
Our Guests
Guest Consultant
Raagini Jawa, MD, MPH

Dr. Raagini Jawa is a Clinical Instructor at Boston University School of Medicine where she practices as an Infectious Disease and Addiction Medicine specialist. She is completing her post-doctoral research fellowship where her work is focused on the intersection of infectious diseases and addition with a focus on harm reduction practices as a mechanism to reduce the rate of infectious complications occurring in people who inject drugs. Her research goals are engaging clinicians in the harm reduction approach and improving humanistic care to persons who use drugs. She provides HIV primary care and addition care for patients at Boston Medical Center and also provides addiction and ID consults in the hospital. Her clinic also offers co-located ID-Addiction care for OPAT and skin-soft tissue infections for patients recently hospitalized for infectious complications of drug use.
Guest Co-Host
Nathan Nolan, MD, MPH

Nathan Nolan is an infectious physician and medical education fellow at Washington University in St. Louis. His practice includes seeing patients in general ID and caring for patients with HIV. He also works within the community with patients who are unhoused and those who struggle with substance use disorder.
Culture
Nathan shared his recent trip to Puerto Rico where he visited a bioluminescent bay. Read more about these here
Raagini’s guilty pleasure is reality TV like 90 Day Fiance re-runs
Consult Notes
Case Summary
35 yo male with history of substance use disorder and untreated hepatitis C who was admitted for fevers and found to have Streptococcus mitis endocarditis
Key Points
A key message from this episode is that your differential for an ill patient in the hospital with comorbid addiction should always have the same differential diagnosis as other patients, but persons who inject drugs are also at increased risk of invasive bacterial and fungal infection.
- In particular, there should be a high index of suspicion for infections that could be introduced hematogenously, such as infective endocarditis, osteomyelitis, septic arthritis, serious skin-soft tissue infection (SSTI), epidural abscess.
- Here is a nice introduction: Marks LR, Nolan NS, Liang SY, Durkin MJ, Weimer MB. Infectious Complications of Injection Drug Use. Med Clin North Am. 2022;106(1):187-200. doi:10.1016/j.mcna.2021.08.006
History & Physical Tips
- A careful substance use history will form the foundation for:
- Immediate medical care of the patient
- Differential diagnosis of potential pathogens to target empiric antimicrobials
- Discussion of harm reduction techniques
- Some notes on a comprehensive history of substances used and preparation steps
- When did you last use drugs? Is the patient on any other medications that may impact the risk of withdrawal?
- How are patients using? They may use other routes other than injection
- What drugs are you injecting? (Opioids only? Other drugs? Many drugs can be injected, such as heroin, fentanyl, cocaine, methamphetamine, ecstasy, ketamine, phencyclidine)
- Environmental contamination of drugs is well described, such as with spore forming bacteria like Clostridia spp which are resistant to heat
- Pathogens can be directly inoculated into the bloodstream if the substance, preparation material, or injection equipment is contaminated with pathogens. Preparation steps may differ and will influence risk of ID syndromes!
- Cooking of drugs? Materials or equipment such as needles, syringes, cookers
- Nonsterile injection technique increases risk of infection with skin flora (Staph, Strep in particular). Less sterile locations such as restrooms raise risk of other organisms such as GI GNRs or Pseudomonas aeruginosa
- Saliva (such as with licking needles) has several oral flora pathogens including Eikenella, Prevotella, viridans group streptococci
- Preparation materials: What is your solvent? Cotton filter, water, acidification agents?
- Raagini spoke a bit about cotton shots in the podcast episode
- Lemon juice is often used as solvent for brown heroin or crack cocaine and can support Candida growth
- Cooking of drugs? Materials or equipment such as needles, syringes, cookers
- Physical or direct injury considerations:
- Where on your body do you inject?
- Skin popping? (transdermal or subcutaneous injection)
- Missed hits?
- What, if any, skin cleaning practices?
- Diving into other possible questions
- Where are you getting your supply from?
- With whom do you use?
- Number of times that you have reused or shared equipment? Shared needles or works can allow transmission of blood borne viral infections such as HIV and Hepatitis B/C
- How do you support their habit? Transactional sex or risky behavior?
- Relevant PMH
- Prior SSTIs or abscesses
- Other serious infections such as endocarditis
- Prior immunocompromising infections, such as HIV
- Prior STIs
- If ever on PrEP
- This is just a start. Also wanted to include two papers from our guest thinking about providing trainees with education on safe injection practice and harm reduction. Training in these conversations provides learners with increased comfort and knowledge and may improve compassion satisfaction
- Jawa R, Saravanan N, Burrowes SAB, Demers L. A call for training graduate medical students on harm reduction for people who inject drugs. Subst Abus. 2021;42(3):266-268. doi:10.1080/08897077.2021.1932697
- Jawa R, Laks J, Saravanan N, Demers L, Wishik-Miller G. Physician trainees’ compassion satisfaction, burnout, and self-efficacy when caring for people who inject drugs. Subst Abus. 2022;43(1):675-681. doi:10.1080/08897077.2021.1986881
As ID docs, isolated pathogens can provide us hints on risk behaviors that patients may be engaging in.
- For example: for patients who isolate oral flora, this is a great place to re-engage with the patient on these IV drug use risk behaviors: licking needles, licking wounds, using saliva as solvent, sharing works, need for cooking longer, skin cleaning, dental hygiene
- Raagini gave another example about Serratia in setting of tap water solvent in the episode. Again, this provides you the opportunity to discuss what harm reduction practices could fit into this patient’s life and how you can help
- Some additional harm reduction practices are described in Table 1 of the Marks, et al. review and you’ll see more in the sections below thinking about reachable moments
It is critical to know not only the ID complications of drug use, but also be able to recognize mimics of other sepsis-like phenomena - like opioid withdrawal!
- It’s important to gather substance use history as noted above
- Dr. Jawa reminded that our patients are experts in their own bodies and have a keen sense of their signs/symptoms of withdrawal from whatever substance they may have chemical dependence on
- For opioid withdrawal:
- Symptoms usually start anywhere from 24-36 hours since last use
- Symptoms can include: diaphoresis, dilated pupils, rhinorrhea, diarrhea, abdominal cramping, nausea, muscle spasms, anxiety, piloerection
- Depending on the type of opioid used, symptoms can intensify with time and last for several days
- It is critical to manage withdrawal concurrently as it helps the patient feel more comfortable, prevents them from seeking to treat themselves, builds a relationship of trust and compassion, and helps the patient and provider see an unclouded picture of the ID syndrome
- Dr. Jawa discussed the approach to ask the patient about their goals of opioid withdrawal management short and long term. A hospitalization for an infection is often a reachable moment and an opportunity for ID docs to engage the patient in harm reduction or treatment with medications for opioid use disorder (MOUD)
- Work with the patient respectfully to give options of comfort medications such as NSAIDs, acetaminophen, hydroxyzine, chlonidine, bentyl; short or long acting opioids, or MOUD such as methadone or buprenorphine-naloxone
- Also, if they are already on MOUD, you need to continue this in order to prevent withdrawal symptoms
- Withdrawal syndrome is separate from pain management! If patient has SUD, it just means that we need to be more mindful of patient’s need for higher potency opioid agonists if they were to need surgical intervention or procedures that require additional pain control
Hospitalizations are reachable moments to engage patients with substance use disorder in treatment, infection prevention, and harm reduction! A presentation for one ID complication should prompt screening for other infections and immunization for vaccine-preventable diseases
- Here is a fantastic resource thinking about opportunities to offer harm reduction: Peckham AM, Young EH. Opportunities to Offer Harm Reduction to People who Inject Drugs During Infectious Disease Encounters: Narrative Review. Open Forum Infect Dis. 2020;7(11):ofaa503. Published 2020 Oct 20. doi:10.1093/ofid/ofaa503
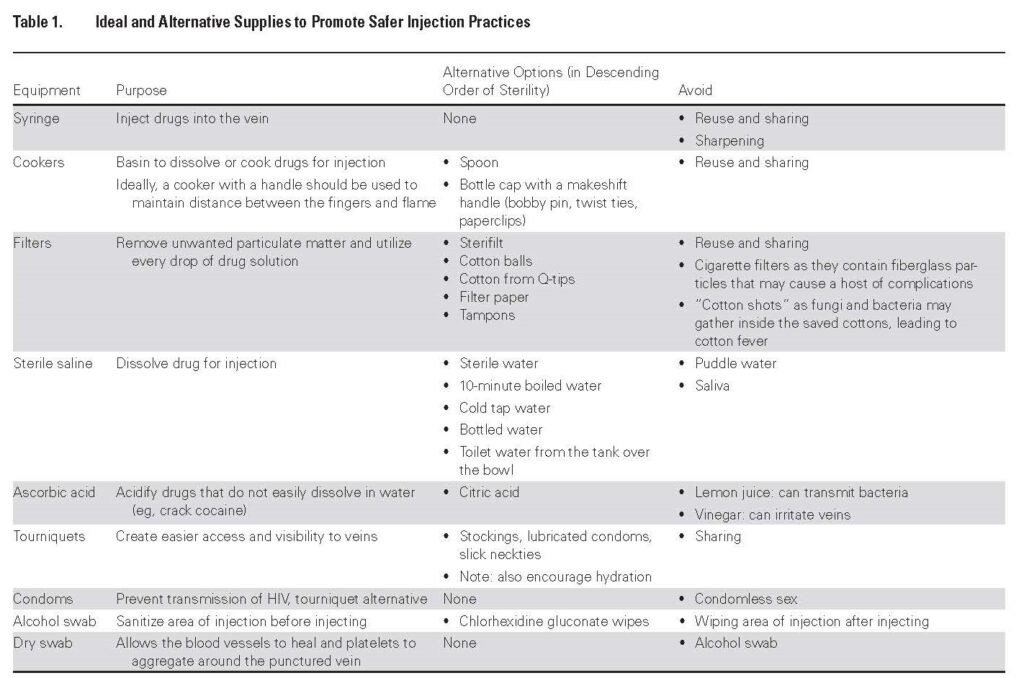
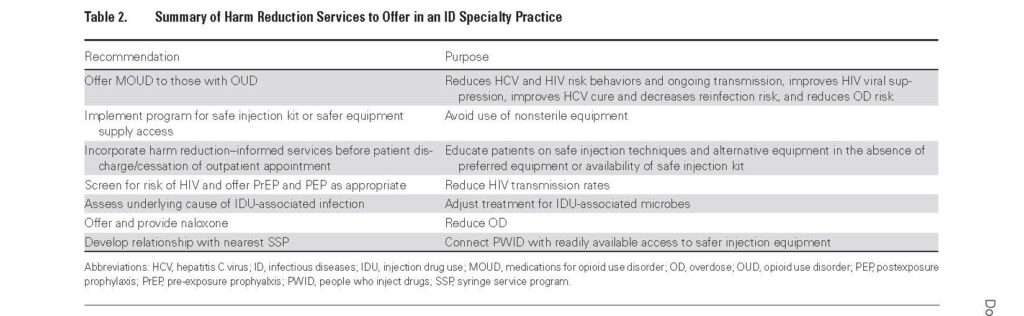
- Check out Table 1 for supplies that promote safer injection practices and Table 2 for a summary of harm reduction services
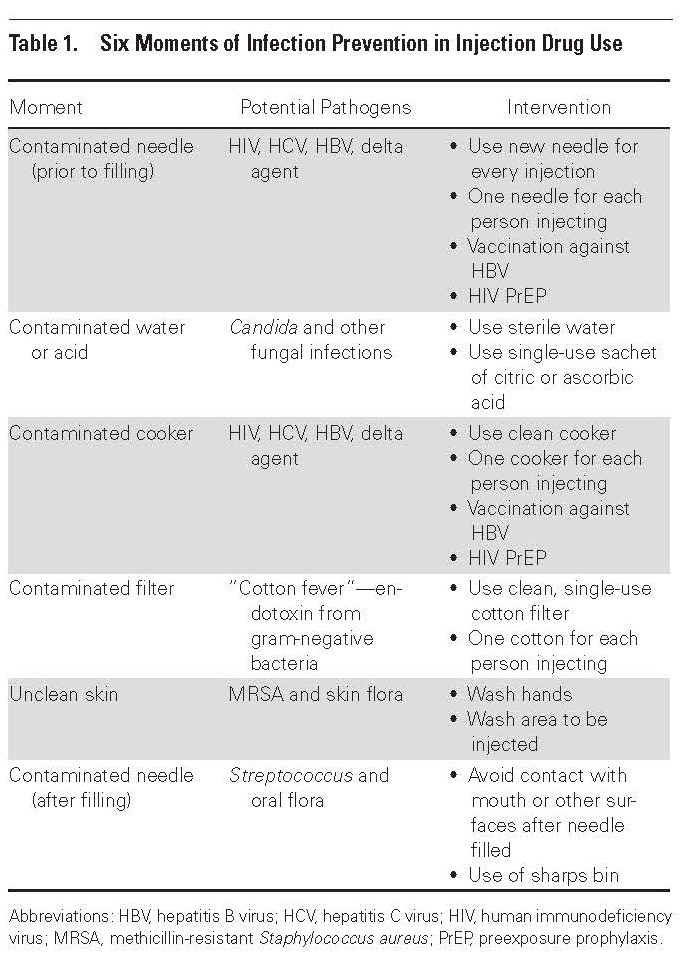
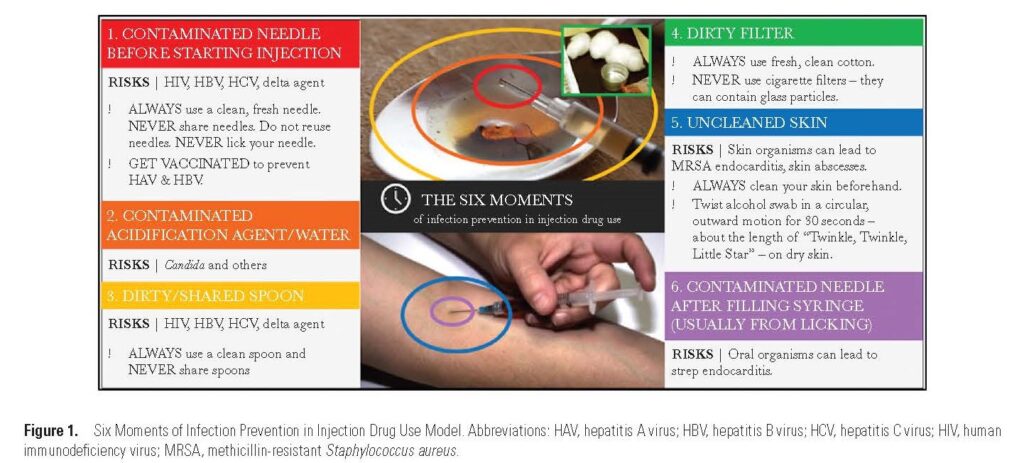
- Here is an educational toolkit for clinicians to use a global (rather than pathogen-specific) infection prevention framework, highlighting the prevention of invasive bacterial and fungal infections: Harvey L, Boudreau J, Sliwinski SK, et al. Six Moments of Infection Prevention in Injection Drug Use: An Educational Toolkit for Clinicians. Open Forum Infect Dis. 2022;9(2):ofab631. Published 2022 Jan 6. doi:10.1093/ofid/ofab631
So we commonly think of practices related to sterile injection equipment or technique, but other considerations to include:
- Linkage with a PCP and any other services they may need!
- Pre- and post-exposure prophylaxis for HIV
- Hepatitis C treatment
- Immunizations, especially Hepatitis B
- STI screening: Marks LR, Reno H, Liang SY, et al. Value of Packaged Testing for Sexually Transmitted Infections for Persons who Inject Drugs Hospitalized With Serious Injection-Related Infections. Open Forum Infect Dis. 2021;8(11):ofab489. Published 2021 Nov 11. doi:10.1093/ofid/ofab489
- For patients who may become pregnant, you can discuss and initiate contraception if desired
- Overdose prevention
Although we didn’t spend too much time on this, just a quick link to the endocarditis components of the case.
- AHA Endocarditis Guidelines are available here
- The POET (partial oral antibiotics for endocarditis) trial is available here
- Here is also one paper looking at evaluation of partial oral antibiotics for PWID: Marks LR, Liang SY, Muthulingam D, et al. Evaluation of Partial Oral Antibiotic Treatment for Persons Who Inject Drugs and Are Hospitalized With Invasive Infections. Clin Infect Dis. 2020;71(10):e650-e656. doi:10.1093/cid/ciaa365
- I liked this recent review on diagnosis and management of infective endocarditis in people who inject drugs: Yucel E, Bearnot B, Paras ML, et al. Diagnosis and Management of Infective Endocarditis in People Who Inject Drugs: JACC State-of-the-Art Review. J Am Coll Cardiol. 2022;79(20):2037-2057. doi:10.1016/j.jacc.2022.03.349
Lastly, we ended with a focus on discharge discussions
- The first step is to attempt to understand why the patient wants to be discharged
- The patients antibiotic plan needs to be made based on their clinical stability – and that means for ID, Addiction, and whatever other needs they may have. We need shared decision making with the patient regarding what treatment plan (IV vs PO vs lipoglycopeptides) is likely to be most effective and fit their lives
- This paper that showed that patients with serious injection drug use-related infections who had patient directed discharges on oral antibiotics had high rates of antibiotic adherence: Lewis S, Liang SY, Schwarz ES, et al. Patients With Serious Injection Drug Use-Related Infections who Experience Patient-Directed Discharges on Oral Antibiotics Have High Rates of Antibiotic Adherence but Require Multidisciplinary Outpatient Support for Retention in Care. Open Forum Infect Dis. 2022;9(2):ofab633. Published 2022 Jan 6. doi:10.1093/ofid/ofab633
- The patients antibiotic plan needs to be made based on their clinical stability – and that means for ID, Addiction, and whatever other needs they may have. We need shared decision making with the patient regarding what treatment plan (IV vs PO vs lipoglycopeptides) is likely to be most effective and fit their lives
- Must-read! Check out this NEJM Curbside Consult from Drs. Ayesha Appa & Joshua Barocas on “Can I Safely Discharge a Patient with a Substance Use Disorder Home with a Peripherally Inserted Central Catheter?” for a great overview! They review literature considering potential PICC complications, combined ID-SUD models, and risk assessment tools for PICC in PWUD
- You can also catch Dr. Appa’s tweetorial here
- The data on PICC complications in persons who use drugs has been mixed, but there is not a contraindication to discharging PWUD with a PICC! Although it might not be the best option for all, there is plenty of evidence that PWUD can safely use PICC for prolonged antibiotics
- While some evidence cited increased vascular complications, there are studies that demonstrate no significant difference in secondary line infections for home based OPAT vs in-hospital care
- Here is a retrospective cohort study from Ontario that found secondary line infection rates and mortality were similar in hospital vs home-based OPAT, suggesting outpatient treatment should be considered in carefully selected patients: Tan C, Shojaei E, Wiener J, Shah M, Koivu S, Silverman M. Risk of New Bloodstream Infections and Mortality Among People Who Inject Drugs With Infective Endocarditis. JAMA Netw Open. 2020;3(8):e2012974. Published 2020 Aug 3. doi:10.1001/jamanetworkopen.2020.12974
- Here is a systematic review of OPAT among PWID that suggests rates of OPAT completion, mortality, and catheter-related complications were comparable to rates among patients without a history of IDU: Suzuki J, Johnson J, Montgomery M, Hayden M, Price C. Outpatient Parenteral Antimicrobial Therapy Among People Who Inject Drugs: A Review of the Literature. Open Forum Infect Dis. 2018;5(9):ofy194. Published 2018 Aug 7. doi:10.1093/ofid/ofy194
- While some evidence cited increased vascular complications, there are studies that demonstrate no significant difference in secondary line infections for home based OPAT vs in-hospital care
- Another big component to homegoing: Paired OPAT and SUD treatment models are important and just make sense!
- This pilot RCT of PICC at home + buprenorphine for opioid use disorder was compared to usual care (hospital) and found 100% completion in both: Fanucchi LC, Walsh SL, Thornton AC, Nuzzo PA, Lofwall MR. Outpatient Parenteral Antimicrobial Therapy Plus Buprenorphine for Opioid Use Disorder and Severe Injection-related Infections. Clin Infect Dis. 2020;70(6):1226-1229. doi:10.1093/cid/ciz654
- Raagini mentioned a paper that she published with colleagues on simulated cost-effectiveness: Adams JW, Savinkina A, Hudspeth JC, et al. Simulated Cost-effectiveness and Long-term Clinical Outcomes of Addiction Care and Antibiotic Therapy Strategies for Patients With Injection Drug Use-Associated Infective Endocarditis. JAMA Netw Open. 2022;5(2):e220541. Published 2022 Feb 1. doi:10.1001/jamanetworkopen.2022.0541
- They found that incorporation of OPAT or partial oral antibiotic approaches along with addiction care services for treatment of patients with IDU-IE was associated with increases in the number of people completing treatment, decreases in mortality, and savings in cost compared with usual care strategy of providing inpatient IV antibiotic therapy alone
- All that being said, PICCs may not be a good option for certain PWUD, just as it may not work for every other patient. Here are a few notes thinking about risk assessment:
- Here is a 9-point assessment focused on delivering OPAT to low risk patients: Eaton EF, Mathews RE, Lane PS, et al. A 9-Point Risk Assessment for Patients Who Inject Drugs and Require Intravenous Antibiotics: Focusing Inpatient Resources on Patients at Greatest Risk of Ongoing Drug Use. Clin Infect Dis. 2019;68(6):1041-1043. doi:10.1093/cid/ciy722
- Here is a description of a case conference used for optimal discharge planning: Sikka MK, Gore S, Vega T, Strnad L, Gregg J, Englander H. “OPTIONS-DC”, a feasible discharge planning conference to expand infection treatment options for people with substance use disorder. BMC Infect Dis. 2021;21(1):772. Published 2021 Aug 9. doi:10.1186/s12879-021-06514-9
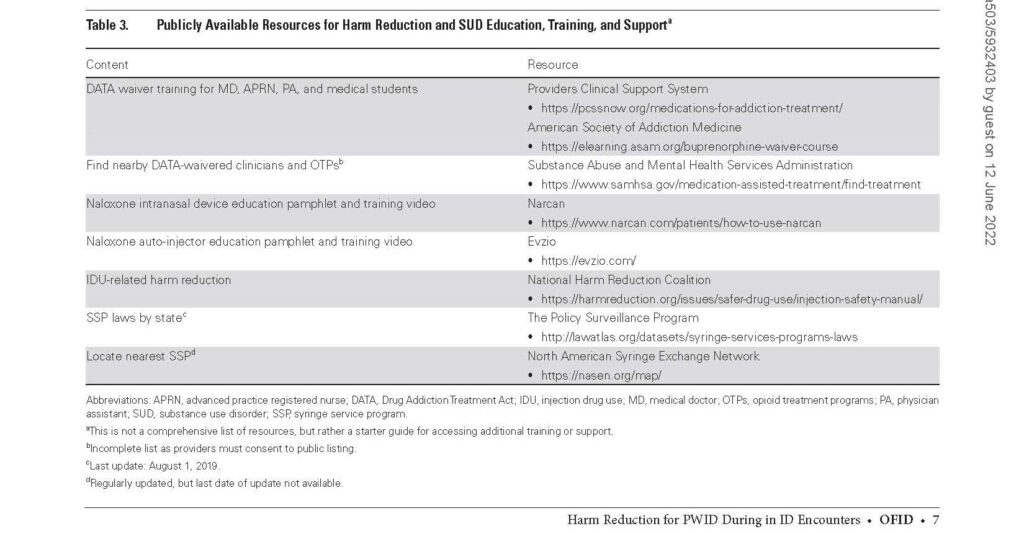
Infographics
Goal
Listeners will be able to approach infections in patients who inject drugs, specifically recognizing the need for harm reduction education, concomitant substance use disorder treatment, and nuanced discharge management plans.
Learning Objectives
After listening to this episode, listeners will be able to:
- To describe how management of substance use disorder is part of holistic care when treating patients who inject drugs with invasive infections
- To discuss the key components of harm reduction counseling when managing patients who inject drugs
- To examine nuanced discharge treatment plans for patients who elect to discharge before completing optimal antibiotic therapy
Disclosures
Our guest (Raagini Jawa) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Jawa, R., Nolan, N., Dong, S. “#46: Reachable Moments”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/1f48b489-2a96-4cf3-a066-7fdca266d046


