Table of Contents
Credits
Host: Sara Dong
Guest: Kruti Yagnik
Writing: Kruti Yagnik, Sara Dong
Producing/Editing/Cover Art/Infographics: Sara Dong
Our Guest
Kruti Yagnik, DO
Dr. Yagnik is an infectious disease staff physician and co-director of antibiotic stewardship at Cleveland Clinic Florida- Indian River Hospital. She completed her infectious disease fellowship at UT Southwestern Medical Center, her internship/residency at the University of Florida, and her medical school education at Nova Southeastern University. She has a particular interest in general infectious diseases, HIV/opportunistic infections, and antibiotic stewardship.
Culture
Some of Kruti’s favorite shows include: Schitt’s Creek, Scrubs, Breaking Bad, Stranger Things, Game of Thrones, The Marvelous Mrs Maisel, and more!.
Consult Notes
Consult Q
Prolonged fever in a frequent traveler
Case Summary
50 year old male frequent traveler who was found to have human African trypanosomiasis
Key Points
Check out the prior episodes and their Consult Notes for more cases in fever in a returning traveler:
Here are some key resources mentioned on the shows (plus a few others!) related to fever in a returning traveler
- CDC Travelers’ Health Page and specific Destination pages
- CDC Yellow Book for health information for international travel
- Global TravEpiNet (GTEN) is a network of travel clinics across the US aimed at improving the health of those traveling internationally. They are supported by CDC
- Christina (episode 48) specifically mentioned Heading Home Healthy, which is a program supported by TravEpiNet, Mass General Hospital, and the CDC. Check out the interactive tool to guide travel counseling here!
- GeoSentinel is a worldwide communication and data collection network for surveillance of travel related morbidity (CDC supports; initiated by International Society of Travel Medicine)
- Travax provides info for travel health, but requires a subscription (your local travel clinic team might have access to this though)
- WHO International Travel and Health resources. Both the CDC and WHO websites are places to look for possible information on outbreaks as well
- Review articles:
- Thwaites GE, Day NP. Approach to Fever in the Returning Traveler. N Engl J Med. 2017;376(6):548-560. doi:10.1056/NEJMra1508435
- Ryan ET, Wilson ME, Kain KC. Illness after international travel. N Engl J Med. 2002;347(7):505-516. doi:10.1056/NEJMra020118
- Gautret P, Parola P, Wilson ME. Fever in Returned Travelers. Travel Medicine. 2019;495-504. doi:10.1016/B978-0-323-54696-6.00056-2
- Fink D, Wani RS, Johnston V. Fever in the returning traveller. BMJ. 2018;360:j5773. Published 2018 Jan 25. doi:10.1136/bmj.j5773
- There are also comprehensive pages through UpToDate that you can reference as well that breaks down clinical approach by the syndrome, incubation period, exposure history and so on
Read more about human African trypanosomiasis in this case!!
This episode covered human African trypanosomiasis (HAT), also known as African sleeping sickness. Let’s start with some of the basics
- A vector-borne infectious disease endemic to sub-Saharan Africa
- It is caused by the protozoan parasite Trypanosoma brucei, which is transmitted by infected tsetse flies (Glossina genus)
- People most exposed to tsetse flies and to the disease live in rural areas and depend on agriculture, fishing, animal husbandry, hunting
- Transmission is usually through a tsetse fly bite but can also rarely include: mother-to-child transmission (crosses placenta), mechanical transmission (through other insects is possible but difficult to assess), accidental in the lab, sexual contact
- Interestingly, there are many regions with tsetse flies that do not have sleeping sickness
- There are 2 forms of the disease caused by different subspecies of the parasite:
- T brucei gambiense (West African trypanosomiasis)
- Endemic to West and Central Africa; has been found in 24 countries
- Accounts for >95% of reported cases
- Causes a slowly progressive / chronic illness
- Person can be infected for months or years without major signs or symptoms of the disease >> when more evidence symptoms emerge, patient is often already in an advanced stage with CNS affected
- T brucei rhodesiense (East African trypanosomiasis)
- Endemic in eastern and southern Africa; has been found in 13 countries
- Causes a more acute illness that evolves over a span of weeks
- Disease rapidly invades the CNS
- T brucei gambiense (West African trypanosomiasis)
- The current disease incidence varies from country to country, and often within different parts of single country
- More recently, >70% of reported cases have occurred in the Democratic Republic of Congo
- You can see the WHO interactive map for HAT here
- Uganda is the only country with both forms of disease, but in separate zones
- This is a very rare diagnosis in returning travelers- The GeoSentinel surveillance network monitors returning travelers and only a single case of T. brucei gambiense HAT was reported among 42 173 ill returning travelers seen between 2007 and 2011
- WHO Fact Sheet
- Büscher P, Cecchi G, Jamonneau V, Priotto G. Human African trypanosomiasis. Lancet. 2017;390(10110):2397-2409. doi:10.1016/S0140-6736(17)31510-6
A few microbiology notes
- CDC DPDx Page with the life cycle image
- In contrast to T.cruzi, these trypanosomes do not have an intracellular phase
- They avoid immune destruction by antibodies by periodically changing their glycoprotein coats through antigenic variation
- Donelson JE. Antigenic variation and the African trypanosome genome. Acta Trop. 2003;85(3):391-404. doi:10.1016/s0001-706x(02)00237-1
Clinical features
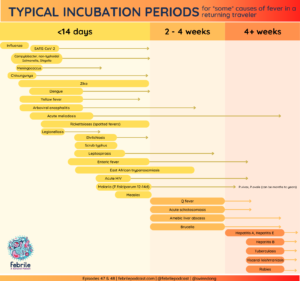
- Incubation periods: rhodesiense HAT is <3 wks but gambiense HAT is variable (ranging from weeks or months)
- The disease has 2 stages:
- A hemolymphatic stage
- Trypanosomes multiply in blood as well as subcutaneous and lymph tissue
- Patients experience fevers, headaches, lymphadenopathy, joint pain, and itching
- The first sign of HAT infection may be the trypanosomal chancre (usually appears ~1 wk after bite; painful, erythematous, indurated, and can ulcerate). Sometimes the clinical presentation is described in 3 phases, including this chancre as the “ulcerative phase”
- Chancres are observed more in travelers than residents of endemic areas
- Followed by
- A meningoencephalitic stage (aka neurological or CNS stage), in which the trypanosomes cross the blood-brain barrier
- Defined by CSF WBC >5 cell/microL with or without trypanosomes in the CSF
- There is an additional subcategory in gambiense HAT of “severe second-stage disease” which was established in the WHO 2019 guidelines (>=100 WBC/microL in CSF +/- trypanosomes in CSF)
- Neurological symptoms typical of the second stage include mental confusion, abnormal behavior, tremor, motor weakness, speech impairment, abnormal gait, seizures, and eventually somnolence
- Disturbance of the sleep cycle is an important feature that gives the disease its name
- A hemolymphatic stage
- This disease (HAT) is considered fatal if left untreated.
- Gambiense has a prolonged early stage whereas the rhodesiense early stage is much shorter
- There is overlap in these clinical manifestations and you can’t distinguish the two stages clinically
- Have you heard of the “Winterbottom’s sign”?
- This describes painless enlarged posterior cervical lymphadenopathy in T.b.gambiense infection
- This is often missed
- What about relapse? Relapse can occur up to 24 mo after completing treatment
- Some references/resources:
- Simarro PP, Franco JR, Cecchi G, et al. Human African trypanosomiasis in non-endemic countries (2000-2010) [published correction appears in J Travel Med. 2012 Mar-Apr;19(2):135]. J Travel Med. 2012;19(1):44-53. doi:10.1111/j.1708-8305.2011.00576.x
- Checchi F, Filipe JA, Haydon DT, Chandramohan D, Chappuis F. Estimates of the duration of the early and late stage of gambiense sleeping sickness. BMC Infect Dis. 2008;8:16. Published 2008 Feb 8. doi:10.1186/1471-2334-8-16
- Checchi F, Funk S, Chandramohan D, Haydon DT, Chappuis F. Updated estimate of the duration of the meningo-encephalitic stage in gambiense human African trypanosomiasis. BMC Res Notes. 2015;8:292. Published 2015 Jul 4. doi:10.1186/s13104-015-1244-3
- Frean J, Sieling W, Pahad H, Shoul E, Blumberg L. Clinical management of East African trypanosomiasis in South Africa: Lessons learned. Int J Infect Dis. 2018;75:101-108. doi:10.1016/j.ijid.2018.08.012
- World Health Organization. Control and surveillance of human African trypanosomiasis. World Health Organ Tech Rep Ser. 2013;(984):1-237.
- Urech K, Neumayr A, Blum J. Sleeping sickness in travelers – do they really sleep?. PLoS Negl Trop Dis. 2011;5(11):e1358. doi:10.1371/journal.pntd.0001358
How is HAT diagnosed?
- The long relatively asymptomatic first stage of T brucei gambiense sleeping sickness is a reason for active screening of populations at risk (to identify at an early stage), but this requires major resources that often are scarce, particularly in remote areas where the disease is usually found
- Definitive diagnosis relies on microscopic visualization of the parasite (Giemsa-stained thick blood smear; smears of chancres or lymph node aspirates; or CSF)
- Serological and PCR testing for HAT exist but are not available in the US. Testing can be sent out and performed at several references laboratories outside of the US
- CATT (card agglutination test for trypanosomiasis) is a fast and sensitive test to screen for T brucei gambiense antibodies in blood, plasma, or serum
- Rapid lateral flow assays
- PCR in blood is highly sensitive and specific.
- A key message from this case and episode = diagnosis and treatment was a multidisciplinary effort with collaboration with the CDC Division of Parasitic Diseases and Malaria & the WHO
- Another point we didn’t talk about quite as much in the episode: staging is very important for all patients suspected of having HAT
- All patients should be screened for CNS involvement with lumbar puncture
Treatment and management of HAT
- Treatment depends on the subspecies of trypanosome and the disease stage >> the earlier disease is identified, the better hope for cure
- Treatment success in the second stage depends on the drugs that cross the blood brain barrier to reach the parasite
- There are WHO guidelines available for treatment from 2019: WHO interim guidelines for the treatment of gambiense human African trypanosomiasis
- You can also read more about the recent updates in this paper: Lindner AK, Lejon V, Chappuis F, et al. New WHO guidelines for treatment of gambiense human African trypanosomiasis including fexinidazole: substantial changes for clinical practice. Lancet Infect Dis. 2020;20(2):e38-e46. doi:10.1016/S1473-3099(19)30612-7
- Significant progress has been made in the development of new oral drugs capable of curing both stages of gambiense HAT
- There are now a total of 6 different drugs available >> which are donated to WHO by manufacturers and distributed free of charge to endemic countries
- In general, medicines available for first-stage disease (hemolymphatic) do not cure second stage (meningoencephalitic) disease. Although effective, those used for second stage disease are not justified for treatment of first stage alone because of their toxicities
- Drugs used in treatment of first stage:
- Pentamidine
- Suramin [adverse effects: nephrotoxicity, allergic reactions]
- Drugs used in treatment of second stage:
- Nifurtimox-eflornithine is typically used as combination therapy (NECT), although both agents can be used as monotherapy
- Regimen for eflornithine is complex and cumbersome, although combination therapy reduced the duration of treatment and number of IV perfusions
- Has not been studied for rhodesiense
- Melarsoprol
- Used for both gambiense and rhodesiense infection
- Many undesirable effects including reactive encephalopathy which can be fatal
- First line treatment for rhodesiense form, but rarely used in gambiense form
- Nifurtimox-eflornithine is typically used as combination therapy (NECT), although both agents can be used as monotherapy
- Drug used in treatment of both stages
- Fexinidazole: newer medication approved in 2018
- Part of the revised WHO protocol as it allowed significant modifications in the management of gambiense cases, such as removing need for systemic LPs for stage and need for injectable treatments in specific patients
- Fexinidazole: newer medication approved in 2018
- In this case, the care team followed the WHO guidelines for treatment of severe disease with nifurtimox-eflornithine
- Treatment was done in coordination with the CDC and via a investigational new drug application
- This was the first time that combination therapy NECT was used for treatment of meningoencephalitic stage of T brucei gambiense HAT in the US
Prevention & Elimination
- Sustained control efforts have greatly reduced the number of new cases, and in recent years (2019, 2020), the number dropped below 10,000 cases for the first time in 50 years
- The WHO has targeted elimination of gambiense HAT transmission as a 2030 target (along with elimination of rhodesiense HAT as a public health problem, meaning no area reporting >=1 case per 10,000 people annually)
- Chemoprophylaxis is not recommended due to the high toxicity of the drugs available
- No vaccine is available to prevent transmission
- Individuals can reduce their risk of acquiring infection by avoiding areas known to harbor infected insects, wearing clothing that reduces biting of the flies, and using insect repellant
- Franco JR, Cecchi G, Priotto G, et al. Monitoring the elimination of human African trypanosomiasis at continental and country level: Update to 2018. PLoS Negl Trop Dis. 2020;14(5):e0008261. Published 2020 May 21. doi:10.1371/journal.pntd.0008261
Other miscellaneous mentions and notes:
- Like textbook references?
- Mandell, Principles and Practice of ID, 8th Ed., 9th Ed.: Chapter 279 Agents of African Trypanosomiasis (Sleeping Sickness)
- Long, Principles and Practice of Pediatric ID, 5th Ed.: Chapter 275 Trypanosoma Species (trypanosomiasis)
- Comprehensive Review of Infectious Diseases
- AAP Red Book
Goal
Listeners will become familiar with human African trypanosomiasis
Learning Objectives
After listening to this episode, listeners will be able to:
- Compare and contrast the clinical presentation of the two forms of human African trypanosomiasis (T. brucei gambiense vs T. brucei rhodesiense)
- Describe the vector, transmission, and geographic distribution for this infection
Disclosures
Our guest (Kruti Yagnik) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Yagnik, K., Dong, S. “#49: Hats Off”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/ff2bc7a0-472c-4e1a-9780-456c618c1229