Table of Contents
Credits
Host(s): Cesar Berto, Sara Dong
Guest: Christina Coyle
Writing: Cesar Berto, Sara Dong
Producing/Editing/Cover Art/Infographics: Sara Dong
Our Guests
Guest Co-Host
Cesar Berto, MD

Dr. Cesar Berto is currently a first year adult infectious diseases fellow in the Massachusetts General / Brigham and Women’s Hospital ID program. He completed his medical school training at Universidad Nacional Mayor de San Marcos Facultad de Medicina San Fernando. He completed residency and chief residency at NYC Health & Hospitals/Jacobi Medical Center, Albert Einstein College of Medicine
Christina Coyle, M.D., M.S.

Christina Coyle, M.D., M.S. is a board-certified physician in Infectious Disease and has practiced Tropical Medicine for over twenty-five years in New York City (NYC). She is a Full Professor in the Department of Medicine and Pathology at the Albert Einstein College of Medicine and is recognized as an expert in Tropical Medicine. She serves as the Director of the Clinical Infectious Disease Service at Jacobi Medical Center, and oversees the largest Tropical Medicine Clinic in the Bronx, NYC. Since 2007, she has been a site director for GeoSentinel, the global surveillance network of the International Society of Travel Medicine (ISTM) and the Centers for Disease Control and Prevention (CDC). Dr. Coyle is currently serving as an associate editor for Open Forum in Infectious Diseases (OFID). From 2016 to 2021, she served as a Member of the American Board of Internal Medicine’s Infectious Disease Exam Committee. Dr. Coyle is widely recognized as an expert on larval tapeworms, neurocysticercosis, and echinococcus, serving on both national and international committees for this disease. Since 2017, she has served on the Echinococcal WHO working group. Dr. Coyle is also a content expert for the Center for Disease and Prevention Control (CDC) for all complicated cases of echinococcus. She is a co-author on “Diagnosis and Treatment of Neurocysticercosis: 2017 Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH).” She is the principal investigator for a CDC cooperative grant, “Reducing the burden of neglected parasitic infections (NPIs) in the United States through evidence-based prevention and control activities”.
Culture
Cesar shared that he recently watched Company, a remade musical by Steven Sondheim.
Christina shared that she is passionate about ballet, dance, and music. She is obsessed with Freddie Mercury from Queen, who once danced with the Royal Ballet.
Consult Notes
Consult Q
Recommendations for work-up of brain calcification
Key Points
What is cysticercosis?
- Cysticercosis is the disease associated with development of the larval stage of the pork tapeworm Taenia solium within an intermediate host
- Clinical syndromes include neurocysticercosis and extraneural cysticercosis
Life Cycle and Transmission
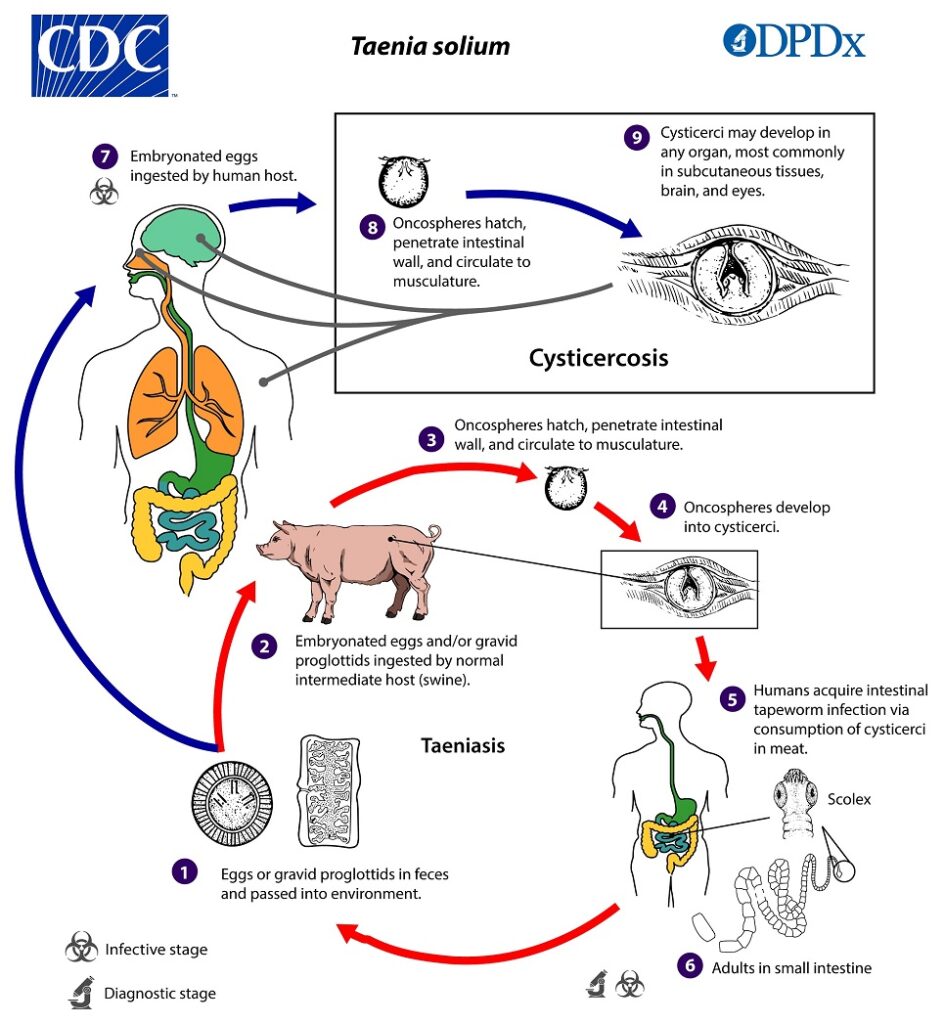
CDC Life Cycle of Taenia solium
- Swine are the usual intermediate host but humans (the usual definitive host) can also serve as accidental intermediate hosts following ingestion of eggs
- Cysticercosis is only acquired from the fecal-oral route (ingestion of eggs), NOT via ingestion of cysticerci in undercooked pork (which is associated with intestinal taeniasis)
- Infected pork contains larval cysts that develop into adult worms in the human intestine but does not contain the eggs that cause cysticercosis
- Some patients with cysticercosis are tapeworm carriers but most individuals with intestinal taeniasis do not develop symptomatic cysticercosis. Human tapeworm carriers are at risk for fecal-oral autoinoculation of eggs though and subsequent development of cysticercosis
- Endemic in many regions of Central and South America, sub-Saharan Africa, India, and Asia
- In countries where cysticercosis is endemic, the prevalence is often higher in rural or periurban areas where pigs are raised and roam free and sanitary conditions are suboptimal (where human fecal contamination of soil is common)
- In these communities, the rate of epilepsy approaches 3% with ~30% of these cases having evidence of cysticercosis
- References/Resources:
- Rajshekhar V, Raghava MV, Prabhakaran V, Oommen A, Muliyil J. Active epilepsy as an index of burden of neurocysticercosis in Vellore district, India. Neurology. 2006;67(12):2135-2139. doi:10.1212/01.wnl.0000249113.11824.64
- Moyano LM, Saito M, Montano SM, et al. Neurocysticercosis as a cause of epilepsy and seizures in two community-based studies in a cysticercosis-endemic region in Peru. PLoS Negl Trop Dis. 2014;8(2):e2692. Published 2014 Feb 13. doi:10.1371/journal.pntd.0002692
- Del Brutto OH, Recalde BY, Mera RM. Incidence of Adult-Onset Epilepsy and the Contributory Role of Neurocysticercosis in a Five-Year, Population-Based, Prospective Study in Rural Ecuador. Am J Trop Med Hyg. 2021;106(1):208-214. Published 2021 Oct 11. doi:10.4269/ajtmh.21-0835
- Lescano AG, Garcia HH, Gilman RH, et al. Taenia solium cysticercosis hotspots surrounding tapeworm carriers: clustering on human seroprevalence but not on seizures. PLoS Negl Trop Dis. 2009;3(1):e371. doi:10.1371/journal.pntd.0000371
Clinical manifestations of cysticercosis
- Tissue cysticerci develop over about 3-8 wks after ingestion of T.solium eggs
- Phases of cysticercosis have been described as:
- Initial (viable) phase: usually asymptomatic, very little inflammation in surrounding tissues, can persist in this stage for years
- Early inflammatory stage
- Degenerating phase
- Nonviable phase
- Christina emphasized that NCC is a pleomorphic disease, and that the clinical presentation is defined by the burden of disease, where disease is located, and the host inflammatory response
- Generally intraparenchymal cysts are associated with seizures and/or headache
- Extraparenchymal cysts are associated with symptoms of elevated intracranial pressure (headaches, nausea/vomiting) +/- altered mental status
- Extraneural cysticercosis may involve a range of tissues but most commonly muscle or subcutaneous tissues
- A few other notes to remember:
- Cysticerci may occur simultaneously in more than one site
- Cysticerci can be at different stages when they present (such as viable vs enhancing vs calcified)
- In the US, most hospitalized patients with NCC present with a single enhancing lesion
Classification of neurocysticercosis
Christina explained that in her opinion, we shouldn’t approach all of neurocysticercosis as one disease – it acts very differently in different spaces of the brain. Here are the general classifications though of NCC disease:
Intraparenchymal NCC:
- Most common form (>60%) of cases
- Onset typically 3-5 years after infection (but can occurs decades later)
- Clinical manifestations depend on the number and location of cysticerci and the degree of associated inflammatory response
- Seizures are the most common clinical manifestation of parenchymal NCC
- Typically focal and may be associated with secondary generalization
- May occur in setting of cyst degeneration (associated with enhancement on radiographic imaging) and/or in setting of nonviable cysticerci (associated with calcification on radiographic imaging)
- In many endemic settings, NCC is most common cause of adult onset seizures
- Less commonly, might have: altered vision, focal neurologic signs, meningitis
- Many parenchymal NCC cases are asymptomatic and identified incidentally via radiographic imaging for other reasons
- Seizures are the most common clinical manifestation of parenchymal NCC
- Prognosis varies with number of cysticeri and degree of inflammation
- Patients with single enhancing lesions have more favorable prognosis than those with multiple viable cysticerci
Extraparenchymal NCC:
- Can occur in ventricles, subarachnoid space, spine, and/or eye
- More common in adults than children
- Symptoms of elevated ICP (HA, nausea, vomiting) +/- altered mental status
- In general, extraparenchymal NCC carries higher risk of complication or death than parenchymal disease
- Intraventricular lesions (free floating cysts in ventricular cavity or attached to choroid plexus) = 10-20% of cases
- Typically symptoms develop when cysticerci lodge in ventricular outflow tracks with consequent obstructive hydrocephalus and increased ICP (gradual or acute onset)
- Headache, nausea, vomiting, altered mental status, decreased visual acuity with papilledema
- Less frequently can see seizures and focal neurologic signs
- Occasionally mobile cysts in third and fourth ventricle can cause intermittent obstruction, leading to episodes of sudden loss of consciousness related to head movements (Bruns’ syndrome)
- Subarachnoid lesions in basilar cisterns is most severe form = ~5% of hospitalized cases
- In some SAN, cysts have lost scolex and may consist of cluster of proliferating membranes (referred to as racemose cysticercosis)
- May be associated with chronic arachnoiditis and/or mass effect due to cyst enlargement
- Spinal lesions ~1% of cases, usually in subarachnoid space where cause inflammatory and demyelinating changes in peripheral nerve roots >> radicular pain, paresthesias, and/or sphincter disturbances
- Orbital and ocular lesions, rare, observed almost exclusively in India
*Extraparenchymal and intraparenchymal disease can coexist*
Diagnosis of neurocysticercosis
- As Christina discussed, the diagnosis of NCC should be based on three columns:
- Patients with seizures and/or manifestations of elevated ICP
- Relevant neuroimaging findings (such as cystic lesions, enhancing lesions, and/or calcifications)
- Relevant epidemiological exposure: is there adequate epi history to support a diagnosis of NCC?
- Diagnosis is based on
- Clinical manifestations
- Neuroimaging findings
- Ideally would include both CT and MRI when feasible
- CT is useful for calcifications, parenchymal cysticerci, and examining eye/orbits
- MRI is useful for detecting relatively small lesions, evaluating degenerative changes, detecting edema, visualizing scolices in calcified lesions
- Findings of intraparenchymal disease include cystic lesions, enhancing lesions, and calcifications – which may all coexist simultaneously
- Identification of a scolex (the end of the tapeworm with suckers and hooks) within cystic lesion is pathognomonic radiographic finding
- Epidemiologic exposure
- Serologic or molecular testing for confirmation
- Antibody tests are most useful for those with consistent neuroimaging findings
- Antibody test of choice = enzyme-linked immunoelectrotransfer blot available from CDC, which is nearly 100% specific to T.solium infection
- Sensitivity varies with the form of NCC and specimen
- Those with multiple parenchymal lesions, ventricular lesions, or subarachnoid lesions, sensitivity of serum testing is nearly 100%
- But those with single parenchymal lesion or calcification only, sensitivity is poor
- Antibody test of choice = enzyme-linked immunoelectrotransfer blot available from CDC, which is nearly 100% specific to T.solium infection
- Antigen detection tests can also be used for follow-up but are relatively limited in the US. CSF antigen tests are more sensitive than serum assays. Antigen testing normalizes with successful treatment
- There are some molecular tests available such as quantitative PCR assay for T.solium
- Antibody tests are most useful for those with consistent neuroimaging findings
- In rare cases, biopsy may be required to differentiate NCC from other brain lesions such as abscess or malignancy
- Christina also reminded us not to forget other additional evaluations including:
- Ophthalmologic exam to exclude ocular disease
- For those who will require corticosteroids, remember appropriate tuberculosis and Strongyloides screening
- Some resources/references:
- Lerner A, Shiroishi MS, Zee CS, Law M, Go JL. Imaging of neurocysticercosis. Neuroimaging Clin N Am. 2012;22(4):659-676. doi:10.1016/j.nic.2012.05.004
- Garcia HH, O’Neal SE, Noh J, Handali S; Cysticercosis Working Group in Peru. Laboratory Diagnosis of Neurocysticercosis (Taenia solium). J Clin Microbiol. 2018;56(9):e00424-18. Published 2018 Aug 27. doi:10.1128/JCM.00424-18
- Vasudevan P, Moorthy RK, Rebekah G, et al. Imaging correlates of serum enzyme-linked immunoelectrotransfer blot (EITB) positivity in patients with parenchymal neurocysticercosis: results from 521 patients. Trans R Soc Trop Med Hyg. 2022;116(2):117-123. doi:10.1093/trstmh/trab091
Management of Taenia solium neurocysticercosis
- Here are some key available resources/guidelines:
- White AC Jr, Coyle CM, Rajshekhar V, et al. Diagnosis and Treatment of Neurocysticercosis: 2017 Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Clin Infect Dis. 2018;66(8):e49-e75. doi:10.1093/cid/cix1084
- WHO guidelines on management of Taenia solium NCC, from 2 Sept 2021
- A major principle is that treatment should target the most severe manifestations of disease
- The initial approach includes managing acute symptoms (such as increased intracranial pressure) and seizures if present
- Management of diffuse cerebral edema >> corticosteroid therapy
- Management of hydrocephalus >> often surgical approach to removal obstructing cysticercus or placement of EVD/shunt
- Management of seizures >> antiepileptic drugs
- Initiation of antiparasitic therapy is never urgent and should only be after consideration of initial symptomatic therapy
- Antimicrobial treatment benefits include faster resolution of active cysts, decreased seizure risk and reduced likelihood of recurrent hydrocephalus
- Risks though include exacerbation of neurologic symptoms due to inflammation around a degenerating cyst
- Antiparasitics should not be used if there is:
- Untreated hydrocephalus
- High cyst burden with diffuse cerebral edema (cysticercal encephalitis)
- Presence of calcified lesions only
- Antiparasitic regimens: Choice depends on burden of disease
- Patient with 1-2 cysts: albendazole
- Patient with 2+ cysts: albendazole and praziquantel
- Duration is typically 10-14 days
- Adjunctive corticosteroids should be given prior to and during antiparasitic therapy
- The dose and duration of the steroid regimen is uncertain and Christina explains her approach in the episode
- Some key references/resources in addition to guidelines above:
- Garcia HH, Pretell EJ, Gilman RH, et al. A trial of antiparasitic treatment to reduce the rate of seizures due to cerebral cysticercosis. N Engl J Med. 2004;350(3):249-258. doi:10.1056/NEJMoa031294
- Otte WM, Singla M, Sander JW, Singh G. Drug therapy for solitary cysticercus granuloma: a systematic review and meta-analysis. Neurology. 2013;80(2):152-162. doi:10.1212/WNL.0b013e31827b90a8
- Kaur S, Singhi P, Singhi S, Khandelwal N. Combination therapy with albendazole and praziquantel versus albendazole alone in children with seizures and single lesion neurocysticercosis: a randomized, placebo-controlled double blind trial. Pediatr Infect Dis J. 2009;28(5):403-406. doi:10.1097/INF.0b013e31819073aa
- Garcia HH, Gonzales I, Lescano AG, et al. Efficacy of combined antiparasitic therapy with praziquantel and albendazole for neurocysticercosis: a double-blind, randomised controlled trial. Lancet Infect Dis. 2014;14(8):687-695. doi:10.1016/S1473-3099(14)70779-0
- Garcia HH, Lescano AG, Gonzales I, et al. Cysticidal Efficacy of Combined Treatment With Praziquantel and Albendazole for Parenchymal Brain Cysticercosis. Clin Infect Dis. 2016;62(11):1375-1379. doi:10.1093/cid/ciw134
Prevention of cysticercosis
Here are a few strategies to consider for targeting stages of transmission:
- Prevent human tapeworm infection to reduce the reservoir of egg carriers:
- Eliminate human consumption of pork contaminated with viable cysticerci >> Christina mentioned how it can be helpful to show patients imaging of pork with cysticerci, which are visible in raw meat (“measly” or “measled” meat)
- Freezing or cooking meat can destroy cysticerci, but pickling and salting will not
- Provide education about routes of transmission and proper hygiene prior to food preparation
- Treating human tapeworm carriers
- Prevent transmission of infections in pigs, such as eliminating access of pigs to human fecal material (disposal of human waste with latrines or sewage systems) and confining pigs so they are not roaming freely [this can be costly though]
Infographics
Goal
Listeners will be able to understand the epidemiology, life cycle, and risk factors for neurocysticercosis
Learning Objectives
After listening to this episode, listeners will be able to:
- Describe the life cycle of Taenia solium
- Describe the typical clinical manifestations and imaging findings of neurocysticercosis
- Discuss the management of neurocysticercosis including antiparasitic medication and corticosteroids
Disclosures
Our guests (Cesar Berto and Christina Coyle) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Coyle, C., Berto, C., Dong, S. “#64: Revenge of the Cyst”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/a9952e58-86f0-476e-8546-547125a7887e