Table of Contents
Credits
Host(s): Rey Perez, Sara Dong
Guests: Andrew Watkins, Jonathan Ryder
Writing: Rey Perez, Jonathan Ryder
Producing/Editing/Cover Art: Sara Dong
Our Guests
Reinaldo (Rey) Perez, MD
Reinaldo Perez, M.D. is a third year Infectious Diseases Fellow at Duke University Medical Center. He works with the Duke Center for Antimicrobial Stewardship and Infection prevention to further their mission of improving patient safety and enhancing quality of care. His research interests include implementation of antimicrobial stewardship interventions and leveraging interprofessional teams. He has additional interests as a medical educator with a passion for curriculum development and effective assessment of educational interventions.
Jonathan Ryder, MD

Jonathan Ryder is an assistant professor in the Division of Infectious Diseases at University of Nebraska Medical Center (UNMC). He serves as an associate medical director of antimicrobial stewardship with interests in diagnostic stewardship and stewardship in rural settings; he also is an associate hospital epidemiologist with the infection control and epidemiology program. Lastly, he has interests in digital medical education and is a co-director of the microbiology block for first-year medical students.
Andrew Watkins, PharmD

Andrew Watkins is an Infectious Diseases pharmacist at St. Dominic Jackson Memorial Hospital in Jackson, Mississippi and serves as the pharmacy stewardship lead for the hospital as well as the Franciscan Missionaries of Our Lady Health System. His responsibilities include prospective audit and feedback, policy and protocol development, implementation of stewardship initiatives, antimicrobial use tracking and reporting, and education of frontline staff on ID- and antimicrobial stewardship-related topics. He also precepts pharmacy residents on antimicrobial stewardship learning experiences.
Culture
- Rey shared the tradition of parrandas, which is a special Puerto Rican tradition of caroling with a bigger and bigger band where you sing at home and they feed you!
- Jonathan shared his Thanksgiving favorites (family, food, and football!), including his favorite dish – sweet potato casserole with pecans on top, no marshmallows
- Andrew loves the holidays as well and is ready to jump into decorations
Consult Notes
Consult Q
This week you’re on call for the hospital’s Antimicrobial Stewardship pager. You receive a call from the cardiac surgery team requesting approval for Daptomycin after a “preoperative urine culture” grew vancomycin resistant Enterococcus faecium in a penicillin allergic patient.
Key Points
This episode celebrates U.S. Antibiotic Awareness Week!
This annual campaign from the Centers for Disease Control and Prevention seeks to highlight the steps everyone can take to improve antibiotic prescribing and use as well as a rallying cry in the fight against increasing antimicrobial resistance. In honor of that, the episode focused on hospital antibiotic stewardship programs. This episode is brought to you in collaboration with the Society of Hospital Epidemiology’s Antimicrobial Stewardship Committee, for which Jonathan is a member.
What are essential components of a stewardship team? Why do we need stewardship teams?
Antimicrobial resistance is a growing problem of international scale. A 2014 report estimated that if antimicrobial resistance trends continued, by 2050 10 million people would die each year from antimicrobial resistance with a global cost up to 100 trillion USD.
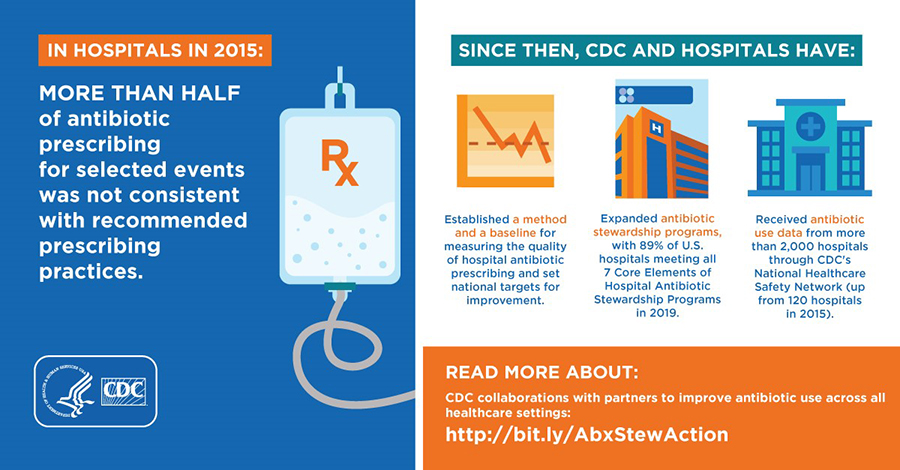
- The primary reasons for inappropriateness included 60% with CAP had excessive durations of therapy and 50% of UTI lacked signs/symptoms of infection.
- We can’t consult on everybody, so we need larger systems-based interventions to improve antimicrobial use in our health systems.
- Along these lines, you have a hard time changing/improving what you don’t track; having a dedicated ASP team really helps with tracking, reporting, and building in accountability to help drive improvements
- Ultimately, antimicrobial stewardship teams are about improving patient care. While there are often downstream health system benefits and contributions to reductions in the larger issue of AMR, the day-to-day often is about optimizing patient care → Making sure each patient has the right drug for the right bug at the right dose for the right duration at the right time
Core elements of hospital antimicrobial stewardship
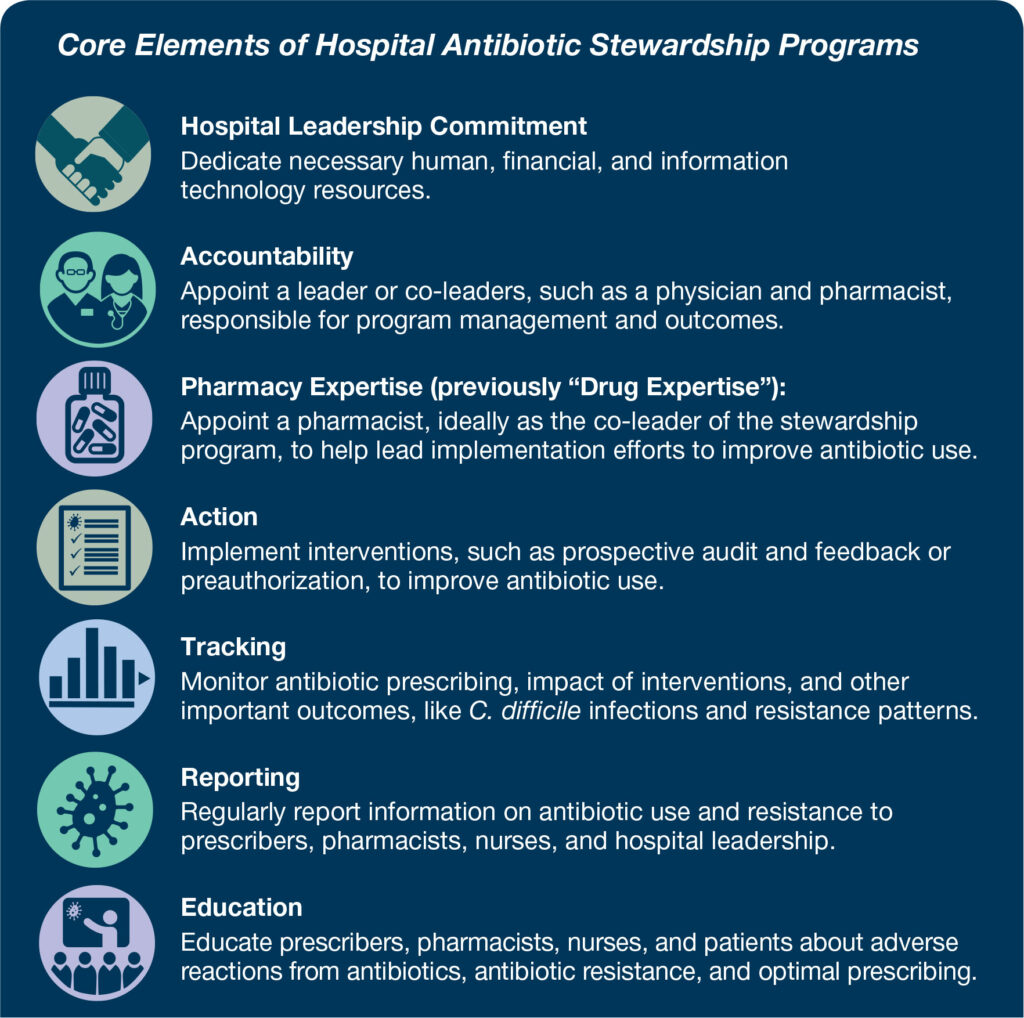
Andrew walked through the core elements of hospital antimicrobial stewardship:
Hospital leadership commitment
- CMS is clear that institutional leadership (along with Quality Improvement) must address issues identified by the IP and ASP committees; open communication between ASP and hospital leadership helps facilitate this (can be periodic meetings, newsletters/emails, etc.)
- Important because bigger initiatives and decisions often flounder or are not possible without leadership support
- Hospitals need to fund these positions for them to be successful and showing the improvements your stewardship work achieves is also a great way to justify your compensation
- Dedicated funding (i.e., salary/pay) and/or dedicated time (i.e., FTE) towards antimicrobial stewardship are great demonstrations of leadership commitment
- Formal statement of support for stewardship is another way to demonstrate leadership commitment
- Numerous templates/examples from CDC and state health departments
Accountability
- A clear leadership structure is essential (typically physician and pharmacist co-leads but can have a single lead)
- Roles should be clarified
- An often overlooked point is that the leader(s) must have education, training, or experience in infectious diseases/antimicrobial stewardship as outlined by TJC/CMS
- Can be “classic” postgraduate training through ID fellowship/ID pharmacy residency or can be through certificate courses plus ongoing CE
Pharmacy expertise
- A pharmacy co-leader of the stewardship program is an essential element
- Because of their positioning in the healthcare system, pharmacists can play a vital role in antimicrobial stewardship.
- Best situated to have access to/track antimicrobial usage data
- Already integrated into the Pharmacy and Therapeutics Committee which provides an avenue for reporting and collaboration with leadership/Quality etc.
- Very familiar with drug-specific information including PK/PD (which can impact dosing optimization and other similar initiatives), drug shortages, formulary information, etc.
- Work closely with providers, nurses, and other disciplines and can help provide education to frontline staff
Action
- Interventions such as prospective audit and feedback or preauthorization
- Facility-specific treatment guidelines are also a key Action and are required by TJC as of this year (at least 2)
- Should be based on national guidelines and literature while taking into account local susceptibility data
- Overall this is the “broadest” of the Core Elements because of the sheer amount of different actions and interventions that can be implemented
- Automatic protocols for renal dosing of abx, IV-to-PO conversions, kinetics-based dosing (great opportunities for pharmacist-driven processes)
- Antibiotic time out processes, “handshake” rounds, automatic stop dates, treatment order sets
- Diagnostic stewardship, microbiology lab partnerships for cascade reporting/“nudging” comments
- Penicillin allergy clarification/challenging/delabeling
- Can be overwhelming at first, but important to use your tracked data to work on 1-2 key things at a time; parlay small wins into bigger changes
Tracking
- Tracking is a vital aspect to any stewardship program because of its utility in identifying opportunities, tracking progress, and building in accountability. There are numerous different metrics that can be tracked, but one of the most important is antibiotic use. Tracking and reporting antibiotic use to NHSN (National Healthcare Safety Network) is actually a regulatory requirement starting in 2024, and it serves as a great method of tracking your use and establishing some benchmarking and comparisons to similar hospitals. This is especially helpful to track in relation to particular initiatives your stewardship group may have implemented to assess impact. CDC has some great examples of using antibiotic use data to identify an opportunity, develop an intervention, and then track progress using data reported to NHSN.
- Tracking can also encompass other aspects such as number/type of A&F patient interventions, which can be helpful for highlighting the impact of your stewardship group and justifying continued or additional funding/positions. You can also track important outcomes such as incidence of C. diff or MDRO infections, etc.
Reporting
- Reporting is often the back end/actionable side of tracking, where you take the data you’ve deemed most important to track and then relay that back to your frontline staff. This increases transparency and buy-in, especially when paired with reporting/education on ongoing initiatives. It also makes the data more actionable and helps with modifying initiatives that may not be having the impact you expected or highlighting early successes. Another great example of reporting is the annual antibiogram, which informs frontline providers on annual resistance rates for commonly seen organisms.
- Overall, the combination of tracking and reporting help drive the stewardship program forward and work as a great accountability piece.
Education
- Education is a very nebulous topic because of all the forms it can take and the numerous audiences it can apply to. It can include education to prescribers, pharmacists, nurses, or patients/family about resistance, the harms of antibiotics, optimal prescribing, etc. Education can take the form of institutional guidelines, antibiograms, hospital policies, in-service presentations, handouts, you name it. Andrew recommended keeping a log of your education sessions so you can easily demonstrate to surveyors who you educated, when, and how/about what. I also recommend making your workflow more efficient by pairing education with other ongoing initiatives or reporting.
Jonathan discussed on Prospective Audit & Feedback as well as Preauthorization
Prospective audit and feedback
- An external review of antibiotic therapy by an expert in antibiotic use, accompanied by suggestions to optimize use, at some point after the agent has been prescribed
- Audit and feedback can be implemented in a variety of ways, depending on the level of expertise available
- The effectiveness of prospective audit and feedback can be enhanced by providing feedback in face-to-face meetings with providers, referred to as “handshake stewardship”
- Pros:
- Provides education through feedback
- Increased autonomy for prescribers (empower teams, more collegial)
- Daytime hours almost exclusively
- May have more broad of an impact evaluating multiple components of antibiotic use (dose, duration, deescalation)
- Cons:
- Can be very resource intensive
- Interventions may occur after several antibiotic doses
- Recommendations are optional for prescribers
Preauthorization
- Requires prescribers to gain approval prior to the use of certain antibiotics
- This can help optimize initial empiric therapy because it allows for expert input on antibiotic selection and dosing, which can be lifesaving in serious infections, like sepsis. It can also prevent unnecessary initiation of antibiotics
- Pros:
- Better control over antibiotic prescribing (especially upfront reduction of unnecessary antibiotics, optimizing initial choice)
- Especially useful for expensive and/or toxic antibiotics or during shortages
- Cons:
- Decreased prescriber autonomy
- Can be adversarial
- Can involve overnight call
- Limited scope to only restricted antibiotics
- Delay in therapy
Being in the preauthorization or prospective audit and feedback roles can be awkward. Unlike a consult where you are being asked for help, you are inserting yourself and sometimes are perceived as the “antibiotic police”. How do you frame your role or what other techniques do you use when giving unsolicited recommendations?
- Share that you are a part of the antimicrobial stewardship team
- Utilize the NARROWS mnemonic (which Jonathan learned from the IDSA’s Antimicrobial Stewardship Training Course”
- N: Name the issue (patient XYZ, calling about the daptomycin)
- A: Ask for the reason (why dapto?)
- R: reflect their emotion (empathize, sick patients, clinical decision making challenging)
- R: Relate with personal experience (I remember when I was on ICU and was worried about a patient)
- O: Orient to suggested management (While daptomycin is an effective therapy, we don’t recommend treating asymptomatic bacteriuria)
- W: Work together on a plan (Do you feel comfortable with discontinuing daptomycin and monitoring for urinary symptoms?)
- S: Set follow-up (call me back if the patient develops new symptoms)
- Jonathan also shared an interesting ethnographic study on differences between how medical teams and surgical teams communicated around antibiotic use
- Medical teams tend to be more “collectivist” in their decision-making, wanting to work together and come to agreed upon plan as a group
- This differed from surgical teams where residents were often making individual decisions as their senior surgeons were not always available to make decisions with the team, given the competing roles in the operating room. Surgical teams also were less likely to have pharmacists available
- Charani E, Ahmad R, Rawson TM, Castro-Sanchèz E, Tarrant C, Holmes AH. The Differences in Antibiotic Decision-making Between Acute Surgical and Acute Medical Teams: An Ethnographic Study of Culture and Team Dynamics. Clin Infect Dis. 2019;69(1):12-20. doi:10.1093/cid/ciy844
How do you decide which intervention to focus on - what is the priority?
- Andrew discussed that prioritization can depend on what has the largest impact and the most manageable / realistic implementation
- In this episode, discussed asymptomatic bacteriuria (ASB) as a targeted initiative which can be tackled from numerous angles such as:
- Education and targeted messaging to highlight the lack of benefit (and risk of harm) in treating ASB
- Reinforce these concepts through patient review and audit&feedback practices reaching out to providers
- Include information in local treatment guidance (which helps the Action Core Element and regulatory requirements)
- Diagnostic stewardship (such as EHR strategies to help with appropriate urine cultures)
- Some resources related to this example:
- Yarrington ME, Reynolds SS, Dunkerson T, et al. Using clinical decision support to improve urine testing and antibiotic utilization. Infection Control & Hospital Epidemiology. 2023;44(10):1582-1586. doi:10.1017/ice.2023.30
- Vaughn VM, Gupta A, Petty LA, et al. A Statewide Quality Initiative to Reduce Unnecessary Antibiotic Treatment of Asymptomatic Bacteriuria. JAMA Intern Med. 2023;183(9):933-941. doi:10.1001/jamainternmed.2023.2749
- Nys CL, Fischer K, Funaro J, et al. Impact of Education and Data Feedback on Antibiotic Prescribing for Urinary Tract Infections in the Emergency Department: An Interrupted Time-Series Analysis. Clin Infect Dis. 2022;75(7):1194-1200. doi:10.1093/cid/ciac073
- Gallegos Salazar J, O’Brien W, Strymish JM, Itani K, Branch-Elliman W, Gupta K. Association of Screening and Treatment for Preoperative Asymptomatic Bacteriuria With Postoperative Outcomes Among US Veterans. JAMA Surg. 2019;154(3):241-248. doi:10.1001/jamasurg.2018.4759
How can you support the stewardship mission?
- Check out one or more of the antimicrobial stewardship certificate programs mentioned during the discussion (SIDP, IDSA, SHEA, MAD-ID, etc)
- Continue building relationships with providers and being a visible group/program within the institution. Everyone benefits when decisions are made collaboratively, and building relationships now opens up more downstream opportunities and enhances conversations.
Infographics
Goal
Listeners will be able to understand the role of antimicrobial stewardship teams
Learning Objectives
After listening to this episode, listeners will be able to:
- List the core elements of hospital antimicrobial stewardship
- Compare and contrast prospective audit and feedback and preauthorization programs
Disclosures
Our guests as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Perez, R., Watkins, A., Ryder, J., Dong, S. “#85: WAAW – Being a Stewie”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/766c9994-1d23-41fc-8482-1d7da368d081