Table of Contents
Credits
Host: Sara Dong
Guest: Brad Cutrell
Writing: Brad Cutrell, Sara Dong
Producing/Editing/Cover Art: Sara Dong
Our Guest
James “Brad” Cutrell, M.D., is an Associate Professor in the Department of Internal Medicine in the Division of Infectious Diseases and Geographic Medicine at UT Southwestern Medical Center in Dallas, TX. He specializes in the care of COVID-19 patients, outpatient parenteral antimicrobial therapy, cardiovascular and orthopedic infections, antimicrobial stewardship, and medical education.
Dr. Cutrell currently serves as the adult ID fellowship program director at UT Southwestern and has a strong interest in medical education, teaching medical students, residents and fellows in infectious diseases. He also leads the antibiotic stewardship program at UT Southwestern Hospital and Clinics in addition to providing clinical care in the UTSW Infectious Disease faculty clinics and ID consult service.
As a COVID-19 treatment and vaccines expert, Dr. Cutrell is advancing COVID-19 research, education, and patient care. His article “Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review” in the Journal of the American Medical Association (JAMA) is one of the most cited articles to date about COVID-19. He is quoted frequently in national and regional media outlets, including The Washington Post, MSNBC, and Bloomberg News, for his knowledge on COVID-19 treatments and vaccines.
Outside of UT Southwestern, he is the former President of the Texas Infectious Diseases Society and serves as a member of several national committees, including the IDSA’s Medical Education Community of Practice Executive Committee, the IDSA In-training Exam Subcommittee and the SHEA’s Journal Club Subcommittee, the latter two of which he chairs. He also serves as one of the faculty moderators for the popular Twitter ID journal club, @IDJClub .
In 2018 and 2019, his peers named him one of the top five doctors in the VA North Texas Health Care System. In 2020, 2021, and 2022, he was voted a D Magazine Best Doctor in infectious diseases, and in 2021 and 2022 he was selected as a Texas Monthly Super Doctors Rising Star. He was also named a Rising Star in the UT Southwestern Leaders in Clinical Excellence awards in 2022.
Outside of medicine, Dr. Cutrell enjoys reading, spending time with his wife and two sons, and traveling.
Culture
Brad shared: Top Gun Maverick; watching the World Cup 2022 with his sons; and The Culture Code by Daniel Coyle
Sara shared: Everything, Everywhere, All at Once; Severance; the After Party; Andor; Crying at H-Mart; Japanese Breakfast
Consult Notes
Match Statistics
- Congratulations and welcome to all of the new and incoming ID fellows! Here’s an update on the breakdown of the match results statistics for appointment year 2023
Adult ID 2023 Appointment | Adult ID 2022 Appointment | Pediatric ID 2023 Appointment | Pediatric ID 2022 Appointment | |
Certified programs | 175 | 172 | 56 | 59 |
Programs filled | 98 (56%) | 70% | 24 (43%) | 41% |
Programs unfilled | 77 (44%) | 32 (57%) | ||
Certified positions | 441 | 436 | 81 | 59 |
Positions filled | 328 (74%) | 82% | 40 (49%) | 41% |
Positions unfilled | 113 (26%) | 41 (51%) |
- NRMP Match Results Statistics, Medicine and Pediatric Specialties – 2022, Overall Statistics
- NRMP Results and Data Specialties Matching Service, 2022 Appointment Year
- We discussed some of the reactions to this year’s match rate. A few of the mentioned published statements:
- IDSA statement from Dr. Carlos del Rio
- STAT News article: “Limits of ‘Fauci effect’: infectious disease applicants plummet, and hospitals are scrambling”
- NPR News article: Newest Doctors shun infectious diseases specialty
- Vox News article: Great News for Germs
A little bit of historical context
- Although the dwindling pipeline into ID become a hot topic after match this year, this has been a more longstanding issue that many have been thinking about and working on for years
- We wanted to offer a bit of a historical context regarding the ID workforce issues
- Here are a few of the quotes mentioned by Brad on the episode:
- 1960s/1970s, Petersdorf predicted the end of ID as a specialty
- Petersdorf RG. The doctors’ dilemma. N Engl J Med. 1978;299(12):628-634. doi:10.1056/NEJM197809212991204
- “Even with my great personal loyalties to infectious disease, I cannot conceive a need for 309 more infectious-disease experts unless they spend their time culturing each other”
- Petersdorf RG. The doctors’ dilemma. N Engl J Med. 1978;299(12):628-634. doi:10.1056/NEJM197809212991204
- Early 1980s
- Petersdorf RG. Whither infectious diseases? Memories, manpower, and money. J Infect Dis. 1986;153(2):189-195. doi:10.1093/infdis/153.2.189
- “in a fee-for- service environment…Infectious disease practitioners have difficulty in making a living. There are few or no procedures. There is a lot of uncompensated phone time, and there is the need to visit several hospitals and spend a good deal of time traveling. In academic medical centers, infectious disease divisions are almost invariably loss leaders, and I know of few that are not heavily supported by university salaries, hospital salaries, and grants. Infectious disease divisions do not earn enough in practice to make a go of it and also require subsidies from the higher-earning divisions in their parent departments”
- Ervin FR. The bell tolls for the infectious diseases clinician. J Infect Dis. 1986;153(2):183-188. doi:10.1093/infdis/153.2.183
- “In 1980 Dr. Paul Beeson outlined that our specialty lacks every attribute needed for successful practice–special technology, chronic disease, and balanced remuneration…the infectious diseases clinician has nothing except cognitive skills for which fair financial awards elude most of us in practice….We are already the least needed of all specialists and future trainees must be honestly informed that infectious disease is a very unwise choice as a field of clinical training. If a cardiologist can say that the “medical profession is more at risk and with more risk factors than a 50 year old man–type A and hypertensive, with CAD who smokes two packs of cigarettes a day and has a cholesterol of 400. Then I would describe our own subspecialty as the same patient with septic shock.”
- Petersdorf RG. Whither infectious diseases? Memories, manpower, and money. J Infect Dis. 1986;153(2):189-195. doi:10.1093/infdis/153.2.189
- In mid-1980s and onward:
- The HIV epidemic spurred new interest in ID practice and research. It also highlighted the growing need for ID workforce to expand. This fueled much of efforts for the better part of 20+ years. Many of the current leaders and luminaries in the field of ID came of age and were inspired to go into ID because of HIV
- In the mid-2000s, trends in total applications to ID downtrended. This year is actually not the worst that it has been.
- Only 42% of programs filled in 2016 match, only 0.7 applicants per position in the NRMP match
- This motivated several actions at the national level, but the most immediate was a move to the “All In Match”, which requires programs to fill all of their available positions through the match rather than offering candidates spots outside of the match
- Analysis of NRMP-SMS Match for ID for 2016-17 Appointment Year and Trends Over Time
- 1960s/1970s, Petersdorf predicted the end of ID as a specialty
So what can we do?! Sara and Brad discussed various topics related to ID workforce in the episode. More on these below
#1 Building the Pipeline: Early exposure to ID in curriculums/rotations and mentorship matters
- Bonura EM, Lee ES, Ramsey K, Armstrong WS. Factors Influencing Internal Medicine Resident Choice of Infectious Diseases or Other Specialties: A National Cross-sectional Study. Clin Infect Dis. 2016;63(2):155-163. doi:10.1093/cid/ciw263
- National cross-sectional mixed-methods study of IM residents graduating from ACGME programs
- First convened focus groups with residents and program directors from 8 residency programs
- Then authors developed questionnaire based on themes from interviews >> disseminated questionnaire to 105 residency programs
- 590 residents responded, ~30% response rate; >40% were international medical grads
- ~⅔ of respondents (and > 70% that applied to ID) recalled developing an interest in chosen field before resident with >20% developing before medical school) >> targeting premedical and medical students is critical component of an approach (which aligns with career decision making trends seen elsewhere in and out of medicine)
- Blyth DM, Barsoumian AE, Yun HC. Timing of Infectious Disease Clinical Rotation Is Associated With Infectious Disease Fellowship Application. Open Forum Infect Dis. 2018;5(8):ofy155. Published 2018 Aug 1. doi:10.1093/ofid/ofy155
- Retrospective study of characteristics of categorical IM interns, staff and fellows they rotated with, and experiential factors of their rotation to determine what predicted future ID fellowship application (all IM interns at Brooke Army Medical Ctr)
- 143 IM interns, 10 (7%) eventually applied to ID
- 90% of those who applied compared to 46% nonapplication to ID >> rotated during the first 6 months of internship (p=0.01)
- IDSA efforts: ID interest groups, ID Week mentorship efforts and attempts to highlight and support trainees at the meeting.
#2 Removing Barriers or Roadblocks: Compensation / debt relief
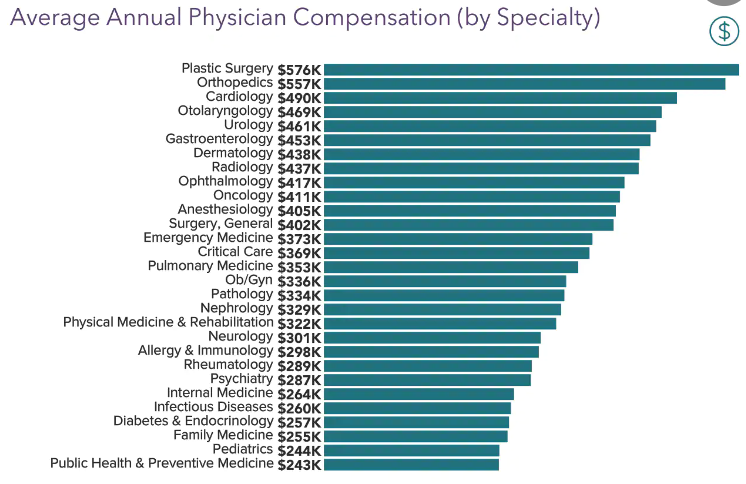
- Most of the focus ends up on remuneration as many surveys demonstrate compensation for average ID doctors are near the bottom of median salary, with pediatric ID usually rounding up of the lowest spots.
- 2022 Medscape survey of annual physician compensation had ID at 260k per year, the lowest for any IM subspecialty and about 100k lower than average for other specialties.
- Pediatric ID even much lower than this
- The sticking point is often that you often will make less than a generalist or other subspecialists >> the “opportunity cost” of additional years of training
- Catenaccio E, Rochlin JM, Simon HK. Differences in Lifetime Earning Potential for Pediatric Subspecialists. Pediatrics. 2021 Apr;147(4):e2020027771. doi: 10.1542/peds.2020-027771. Epub 2021 Mar 8. PMID: 33685988.
- Work on the IDSA / society level regarding compensation
- ID Physician Compensation Initiative
- Compensation Negotiation Playbook
- Webinar series
- BIO Preparedness Workforce program, included in PREVENT Pandemics Act
- ID Physician Compensation Initiative
- A lot of focus gets placed on the salary component, but we emphasized that there are conflicting results on why trainees ultimately do not choose careers in ID. In compensation surveys, usually at least half of ID physicians do feel fairly compensated
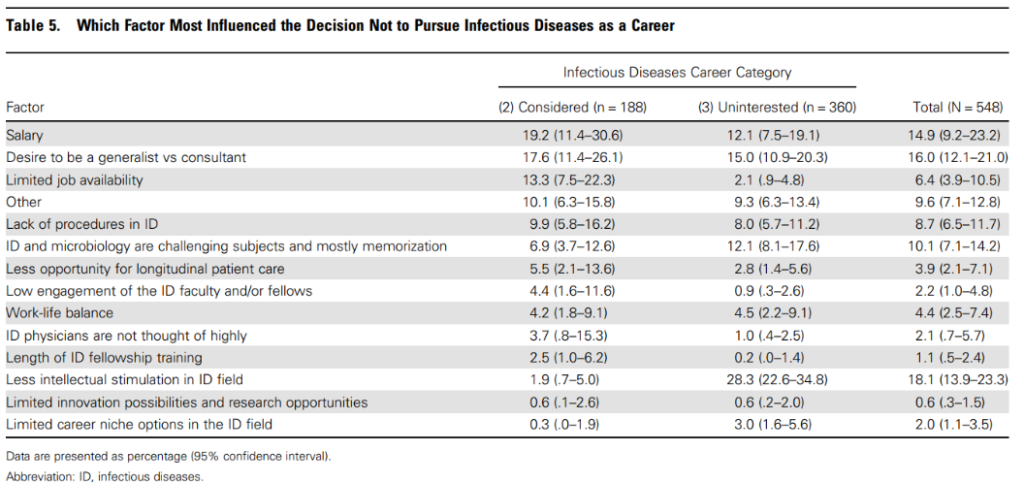
- Barsoumian AE, Hartzell JD, Bonura EM, Ressner RA, Whitman TJ, Yun HC. Factors Influencing Selection of Infectious Diseases Training for Military Internal Medicine Residents. Clin Infect Dis. 2018;67(10):1582-1587. doi:10.1093/cid/ciy322
- For those who considered ID, 73% changed mind in PGY2 or PGY3 year and cited:
- Salary (22%)
- Lack of procedures (18%)
- Training length (18%)
- For those who considered ID, 73% changed mind in PGY2 or PGY3 year and cited:
- Barsoumian AE, Hartzell JD, Bonura EM, Ressner RA, Whitman TJ, Yun HC. Factors Influencing Selection of Infectious Diseases Training for Military Internal Medicine Residents. Clin Infect Dis. 2018;67(10):1582-1587. doi:10.1093/cid/ciy322
#3 Fundamental change in healthcare market dynamics
Another viewpoint is one that is expressed by Brad Spellberg, which he published as Perspective in OFID in 2020: Alignment with Market Forces: The “Re-Whithering” of ID
- “The answer is very simple. The field of ID has never adapted to the reality of market forces.”
- “One of the predominant handicaps of the ID clinical specialty is that there is nothing we do that no one else can do. Only Oncologists prescribe cancer chemotherapy. Only Cardiologists do cardiac caths. Only Surgeons take patients to the operating room. What is it that only ID practitioners do?”
- Arguments here: We need to change the interaction between our specialty and the healthcare system so that ID work is aligned with market forces >> legal and/or regulatory changes
- #1: Only those who have undergone specialized ID training, whether by accredited training or certification course, should be allowed (eg via law, regulation or medical staff credentialing) to interpret diagnostic / susceptibility results or prescribe newly approved antimicrobial agents
- #2: push to mandate public reporting of antimicrobial prescriptions at the system level and link pay for performance measures to such reporting (systems that use at high end adjusted for dz severity, should receive payment penalties vs lower end receiving payment bonuses)
- #3: push for true reform in payment structure of our US healthcare system. Cognitive specialists who keep people from becoming sick and minimize waste/harm become more valuable to payers than those that conduct expensive procedures in patients are are already sick
- Read the full paper here: Spellberg B. Alignment With Market Forces: The “Re-Whithering” of Infectious Diseases. Open Forum Infect Dis. 2020;7(8):ofaa245. Published 2020 Jun 20. doi:10.1093/ofid/ofaa245
Other thoughts/special populations that need attention
This is not an exhaustive list and only scratches the surface — but here are some notes from additional topics covered in the episode:
- Need for legislation around international medical graduates (IMG) support for waiver jobs
- More awareness in information and action steps about visa process
- Access to resources and immigration lawyers
- State and national advocacy for increase in visa-waiver jobs
- Pediatric ID
- Growth in pediatric medical subspecialty workforce pipeline has also been a longstanding issue and concern that many people want to understand a bit better
- There was a paper from 2021 that took a look at the pediatric subspecialty workforce and found that although the # of individuals entering fellowship training increased, it was uneven. They compared the fields with greatest growth and noted those with limited growth – which peds ID was one of (along with nephrology, adolescent, child abuse)
- Macy ML, Leslie LK, Turner A, Freed GL. Growth and changes in the pediatric medical subspecialty workforce pipeline. Pediatr Res. 2021;89(5):1297-1303. doi:10.1038/s41390-020-01311-7
- Many of the concerns are ones we’ve already expressed earlier: Prolonging your training. Concern for amount of debt and lower salaries that come with additional training
- PIDS also supports similar advocacy efforts regarding compensation and debt relief
- Pediatric Subspecialty Loan Repayment Program
- Pathways to careers in pediatric ID – SUMMERS program, trying to expose early learners
- meetID (Mentored, Engaging, Educational, Trainee-Focused) program
- Some additional challenges: job market, lack of research funding
- Impact of combined fellowships? FYI to audience that the Medicine & Pediatric Specialties match was combined for the first time this year – which at least helps facilitate for some of the combined options. Anecdotally it seems that people find this has been a positive impact, particularly on pediatric side, if we can support excellent candidates in creating these opportunities
- Growth in pediatric medical subspecialty workforce pipeline has also been a longstanding issue and concern that many people want to understand a bit better
- Physician Scientist workforce
- Some of the same challenges but also unique aspects to consider such as: increased collaboration and funding for federal and university grant funding. Additional mentor support for early ID physician scientists, expanding K awards to cover more translational and public health work, etc.
- Singh U, Levy J, Armstrong W, et al. Policy Recommendations for Optimizing the Infectious Diseases Physician-Scientist Workforce. J Infect Dis. 2018;218(suppl_1):S49-S54. doi:10.1093/infdis/jiy246:
- Diversity, Equity, Inclusion efforts
- Dismal number of URiM fellow presentation on pediatric side. Check out some of the resources below and the JPIDS Supplement Dec 2022 Eliminating Health Disparities in Pediatric ID
- Tanya Rogo, Sabina Holland, Magali Fassiotto, Yvonne Maldonado, Tuhina Joseph, Octavio Ramilo, Katrina Byrd, Shirley Delair, Strategies to Increase Workforce Diversity in Pediatric Infectious Diseases, Journal of the Pediatric Infectious Diseases Society, Volume 11, Issue Supplement_4, December 2022, Pages S148–S154, https://doi.org/10.1093/jpids/piac094
- Anthony R Flores, Tina Q Tan, Kristina A Bryant, Creating a Diverse and Inclusive Pediatric Infectious Diseases Workforce, Journal of the Pediatric Infectious Diseases Society, Volume 11, Issue Supplement_4, December 2022, Pages S125–S126, https://doi.org/10.1093/jpids/piac103
- Yeh SH, Vijayan V, Hahn A, et al. Profile of the Pediatric Infectious Disease Workforce in 2015 [published correction appears in J Pediatric Infect Dis Soc. 2019 Jul 1;8(3):287]. J Pediatric Infect Dis Soc. 2019;8(1):29-38. doi:10.1093/jpids/pix094

But what can we do on an individual basis to recruit into ID? Share #WhyID!
10. You are a medical detective and an internist’s internist
9. You are the hospital’s social butterfly
8. You get to make the social history relevant again
7. You get to help people you never even meet
6. You don’t have to choose between being a specialist and a generalist
5. The world is your oyster
4. You will never be bored because your work is constantly evolving
3. You get to play with cool new toys
2. You will save patients’ lives and be well positioned to lead in an era of value-based care
1. You join a community that loves what they do and passionately advocates for all patients no matter what
A few other miscellaneous links
- Fauci AS, Morens DM. The perpetual challenge of infectious diseases [published correction appears in N Engl J Med. 2012 Mar 1;366(9):868]. N Engl J Med. 2012;366(5):454-461. doi:10.1056/NEJMra1108296
- Fauci AS. It Ain’t Over Till It’s Over … but It’s Never Over – Emerging and Reemerging Infectious Diseases. N Engl J Med. 2022;387(22):2009-2011. doi:10.1056/NEJMp2213814
- JID Supplement from 2017: Careers in Infectious Diseases
- Walensky RP, Del Rio C, Armstrong WS. Charting the Future of Infectious Disease: Anticipating and Addressing the Supply and Demand Mismatch. Clin Infect Dis. 2017;64(10):1299-1301. doi:10.1093/cid/cix173
- Mike Angarone’s 2 cents: https://sites.northwestern.edu/nuidfellowship/2022/12/14/my-2-cents-on-the-2022-id-match/
Disclosures
Our guest (Brad Cutrell) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Cutrell, B., Dong, S. “#65: Match Update & #WhyID”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/046af2db-8401-48fb-bef9-a58a0b1b2f57