Table of Contents
Credits
Hosts: Katie Sharma, Sara Dong
Guests: Amalia Aldredge, Varun Phadke
Writing: Katie Sharma, Amalia Aldredge, Varun Phadke, Sara Dong
Producing/Editing/Cover Art: Sara Dong
Infographics: Sara Dong
Our Guests
Guest Co-Host
Katie Sharma, MD

Dr. Katie Sharma is a fourth-year medical student at Emory University School of Medicine, who recently matched at Emory for internal medicine residency. She graduated from Georgia Tech in 2010 with a business degree and began a career in healthcare consulting and analytics, eventually pivoting to pursue medicine. Katie’s interest in infectious diseases was initially piqued by the fantastic ID medical educators at Emory (::cough cough:: Dr. Phadke) who gave lectures on various ID topics during her pre-clinical years. When she is not at the hospital, she is with her husband, Abhi, chasing around their three- year-old son, Grady.
Guest Discussant
Amalia Aldredge, MD

Dr. Amalia Aldredge is originally from Seattle, but moved to Atlanta for IM residency at Emory and stayed there for additional training, where she is currently a second-year Infectious Diseases fellow. She is interested in disparities in HIV care, HIV prevention including novel ways to deliver care, and medical education. In her free time, she loves hiking with her dog, baking (current favorites are the brown butter sage sablés from Dessert Person), and binge-reading novels.
Guest Discussant
Varun Phadke, MD

Dr. Varun Phadke, who you might remember from episode #26 on culture negative endocarditis. Varun earned his MD degree from Harvard Medical School and completed his residency training at New York-Presbyterian Hospital / Columbia University Medical Center. He then moved to Atlanta for his ID fellowship training and has been on Emory faculty since that time. He serves as the Associate Program Director for the ID fellowship program, a core faculty member for the IM residency program, and is the Assistant Vice Chair of Education for Clinical Reasoning. He previously completed a fellowship in diagnostic excellence through the Society to Improve Diagnosis in Medicine and is passionate about teaching clinical reasoning. I will also point out that he was the IDSA Medical Education Community of Practice Featured Educator for 2/1/23!
Culture
Katie mentioned Ikebana, Japanese flower arranging
Amalia shared some of her adventures in beekeeping
Varun shared a podcast called The Moth and the book How to Tell a Story
Consult Notes
Consult Q
55-year-old man presents with fever and altered mental status
Case Summary
55 year old male with HTN and DM who presents with acute change in mental status and is found to have Strep pneumoniae meningitis
Key Points
This episode was a bit unique because one of our discussants also used the teaching portion of the case to point out:
- How to ask good questions
- How to probe (and correct/refine) clinical reasoning in real-time
- How to foster progressive problem solving
Amalia gave a great differential diagnosis considering a patient who presented with altered mental status. These Consult Notes will focus on several of the learning points regarding CSF interpretation and bacterial meningitis. Let’s start by discussing clinical features of bacterial meningitis
- Patients with bacterial meningitis are generally quite sick and present quickly, although ultimately the tempo of illness is impacted by both host and microbial factors
- The typical described features include:
- Fever
- Nuchal rigidity / stiff neck
- Change in mental status, typically suddenly
- Severe headache
- Other manifestations might include seizures, aphasia, cranial nerve palsy, rash
- Assessing for meningeal irritation is important and patients may not complain specifically of stiff neck. Here are some signs/tests to illustrate meningismus you might remember or use:
- Passive or active flexion of neck with inability to touch chin to chest
- Brudzinski sign: spontaneous flexion of hips during attempted passive flexion of neck
- Kernig sign: inability or reluctance to allow full extension of knee when hip is flexed 90 degrees (usually perform in supine position)
- Jolt accentuation of headache: headache worsens with horizontal rotation of head at a frequency of 2-3 times per second
- Here is a nice resource thinking about the physical exam and acute meningitis:
- Attia J, Hatala R, Cook DJ, Wong JG. The rational clinical examination. Does this adult patient have acute meningitis?. JAMA. 1999;282(2):175-181. doi:10.1001/jama.282.2.175
- There is an update to this with evidence through 2004 in the book: Hatala R, Attia J, Wong JG. The Rational Clinical Examination: Evidence-Based Clinical Diagnosis. Does this adult patient have acute meningitis? Update. McGraw Hill, 2009. 403-406.
- Ultimately no one symptom or maneuver can totally exonerate meningitis!
- Resources:
- van de Beek D, Brouwer M, Hasbun R, Koedel U, Whitney CG, Wijdicks E. Community-acquired bacterial meningitis. Nat Rev Dis Primers. 2016;2:16074. Published 2016 Nov 3. doi:10.1038/nrdp.2016.74
- van de Beek D, de Gans J, Spanjaard L, Weisfelt M, Reitsma JB, Vermeulen M. Clinical features and prognostic factors in adults with bacterial meningitis [published correction appears in N Engl J Med. 2005 Mar 3;352(9):950]. N Engl J Med. 2004;351(18):1849-1859. doi:10.1056/NEJMoa040845
The initial approach when you suspect bacterial meningitis includes obtaining a lumbar puncture (LP). CSF testing should be sent for:
- Cell count and differential
- Protein
- Glucose
- Bacterial culture and Gram stain
- Other tests as appropriate, such as:
- CSF HSV PCR
- In certain patients, may send special tests such as CSF CrAg or fungal/AFB cultures
- Multiplex PCR like BioFire meningitis/encephalitis panel (if available)
- Sending/saving an extra tube of CSF for additional studies are helpful in case the clinical course warrants additional testing
As discussed on the episode, you can have challenges with multiplex PCR panels
- False negatives ~1.5%
- If you suspect a particular pathogen and it is available, use a singleplex PCR. Other tests may be necessary for specific pathogens (such as cryptococcal antigen)
- Overall decent negative predictive value
- False positives ~4%
- You risk learning about a positive that is clinically insignificant in your patient (such as HHV6)
- S.pneumoniae is the most common false positive pathogen
Interpreting CSF profiles!
- Characteristic findings in bacterial meningitis:
- CSF WBC count >1000, usually with neutrophilic predominance
- CSF glucose concentration <40 mg/dL
- CSF protein concentration >200 mg/dL
- We’ll have an infographic comparing/contrasting the typical CSF findings in various CNS infections
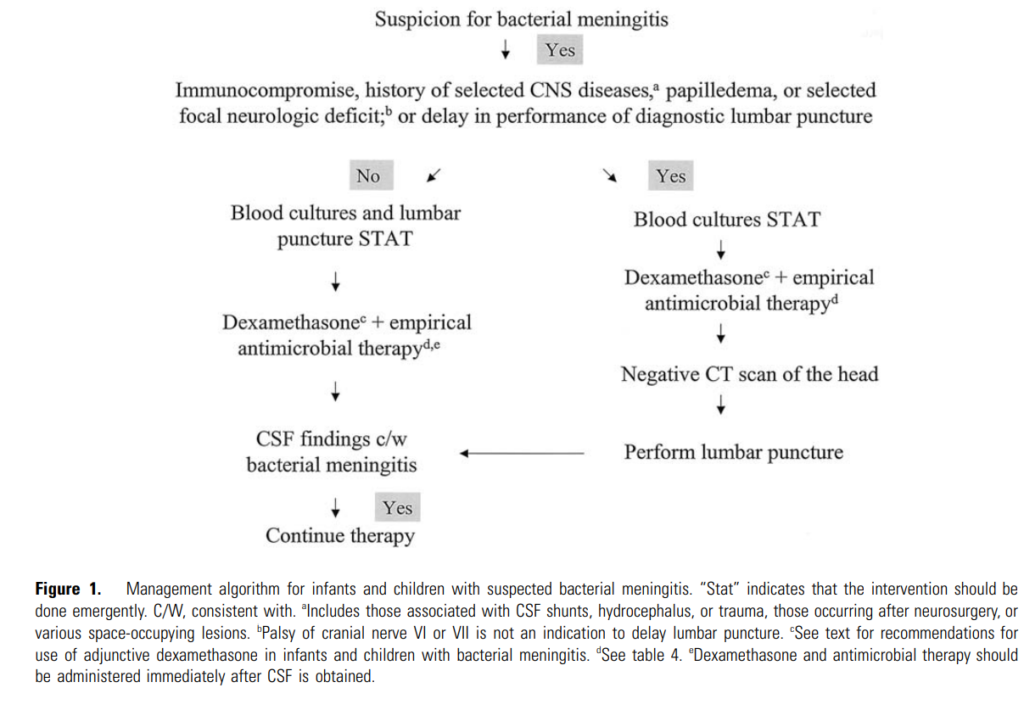
What sequence of testing and treatment should be recommended? Which patients should have head CT before LP? When should antibiotics +/- steroids be given?
- After LP, there is a mild transient lowering of lumbar CSF pressure (due to removal of CSF and continued leakage of CSF from opening made in arachnoid membrane that is rapidly communicated throughout subarachnoid space)
- In patients with intracranial, space-occupying lesions >> there is a relative pressure gradient with downward displacement of cerebrum and brainstem that can be increased by LP >> risking precipitating brain herniation
- So CT is used to exclude occult mass lesion or other findings that could lead to cerebral herniation during CSF removal
- So who should have a head CT first? Generally those with one or more of the risk factors below:
- Immunocompromised state (such as HIV infection, immunosuppressive therapy, solid organ or hematopoietic cell transplant)
- History of CNS disease such as mass lesion, stroke, or focal infection
- Papilledema
- New-onset seizure within one week of presentation
- Abnormal level of consciousness
- Focal neurologic deficit
- Hasbun R, Abrahams J, Jekel J, Quagliarello VJ. Computed tomography of the head before lumbar puncture in adults with suspected meningitis. N Engl J Med. 2001;345(24):1727-1733. doi:10.1056/NEJMoa010399
- You can review the IDSA guidelines (a bit old now): Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(9):1267-1284. doi:10.1086/425368
- Here is the summary management algorithm from the IDSA guidelines noted above:
- A few other meningitis guidelines:
- van de Beek D, Cabellos C, Dzupova O, et al. ESCMID guideline: diagnosis and treatment of acute bacterial meningitis. Clin Microbiol Infect. 2016;22 Suppl 3:S37-S62. doi:10.1016/j.cmi.2016.01.007
- McGill F, Heyderman RS, Michael BD, et al. The UK joint specialist societies guideline on the diagnosis and management of acute meningitis and meningococcal sepsis in immunocompetent adults [published correction appears in J Infect. 2016 Jun;72 (6):768-769]. J Infect. 2016;72(4):405-438. doi:10.1016/j.jinf.2016.01.007
- One of the key principles of bacterial meningitis management is to initiate therapy as quickly as possible after LP (or as quickly as possible after blood cultures obtained if planning for CT head)
- If a head CT is indicated >> Obtain blood cultures immediately and start empiric antimicrobial therapy (and dexamethasone if using) prior to head CT
- If no risk factors, obtaining a head CT has no clinical benefit and delays LP >> so obtain blood cultures and LP as soon as possible and then start dexamethasone and antibiotics
- Delay in administration of antibiotics impacts mortality and residual neurological defects!
- Auburtin M, Wolff M, Charpentier J, et al. Detrimental role of delayed antibiotic administration and penicillin-nonsusceptible strains in adult intensive care unit patients with pneumococcal meningitis: the PNEUMOREA prospective multicenter study. Crit Care Med. 2006;34(11):2758-2765. doi:10.1097/01.CCM.0000239434.26669.65
- Aronin SI, Peduzzi P, Quagliarello VJ. Community-acquired bacterial meningitis: risk stratification for adverse clinical outcome and effect of antibiotic timing. Ann Intern Med. 1998;129(11):862-869. doi:10.7326/0003-4819-129-11_part_1-199812010-00004
- Bodilsen J, Dalager-Pedersen M, Schønheyder HC, Nielsen H. Time to antibiotic therapy and outcome in bacterial meningitis: a Danish population-based cohort study. BMC Infect Dis. 2016;16:392. Published 2016 Aug 9. doi:10.1186/s12879-016-1711-z
- Køster-Rasmussen R, Korshin A, Meyer CN. Antibiotic treatment delay and outcome in acute bacterial meningitis. J Infect. 2008;57(6):449-454. doi:10.1016/j.jinf.2008.09.033
- Proulx N, Fréchette D, Toye B, Chan J, Kravcik S. Delays in the administration of antibiotics are associated with mortality from adult acute bacterial meningitis. QJM. 2005;98(4):291-298. doi:10.1093/qjmed/hci047
- Lepur D, Barsić B. Community-acquired bacterial meningitis in adults: antibiotic timing in disease course and outcome. Infection. 2007;35(4):225-231. doi:10.1007/s15010-007-6202-0
- Resources:
- Park N, Nigo M, Hasbun R. Comparison of Four International Guidelines on the Utility of Cranial Imaging Before Lumbar Puncture in Adults with Bacterial Meningitis. Clin Neuroradiol. 2022;32(3):857-862. doi:10.1007/s00062-022-01143-4
- Salazar L, Hasbun R. Cranial Imaging Before Lumbar Puncture in Adults With Community-Acquired Meningitis: Clinical Utility and Adherence to the Infectious Diseases Society of America Guidelines. Clin Infect Dis. 2017;64(12):1657-1662. doi:10.1093/cid/cix240
What empiric antibiotics should be selected for suspected bacterial meningitis? What is the typical microbiology of bacterial meningitis?
- The empiric regimen for meningitis is a reflection of the common bacterial pathogens, which vary by age
- We’ll be putting together an infographic on this!
- Remember that S.pneumoniae and N.meningitidis are the two most commonly isolated pathogens for community-acquired bacterial meningitis in adults
- Selected third generation cephalosporins (such as ceftriaxone) are the beta-lactams of choice in empiric meningitis treatment due to consistent CSF penetration and potent activity against major pathogens of bacterial meningitis
- The exceptions? L.monocytogenes and some penicillin-resistant strains of S.pneumoniae
- In the US, vancomycin is added as empiric treatment due to prevalence of ceftriaxone resistant >1% until culture and susceptibility results are available
- Ceftazidime is less active against penicillin-resistant pneumococci than ceftriaxone
- In the show, Varun and Amalia discussed how you might think about a different regimen in those patients with beta-lactam allergies:
- A good reference is the available chart in UpToDate for quick reference
- We will save health-care associated / post-neurosurgical CNS infections for a future episode, but just a quick note to emphasize that the “usual” antibiotics would not be the best option because the major causes are different
- We empirically treat for extra bugs in this setting: MRSA (vanc) + Pseudomonas (cefepime/ceftaz/mero)
- Cultures are very important
- A link to the IDSA guidelines for ventriculitis/meningitis/shunt infections: Tunkel AR, Hasbun R, Bhimraj A, et al. 2017 Infectious Diseases Society of America’s Clinical Practice Guidelines for Healthcare-Associated Ventriculitis and Meningitis. Clin Infect Dis. 2017;64(6):e34-e65. doi:10.1093/cid/ciw861
- Sometimes, intrathecal antibiotics are considered if clinical failure on appropriate antibiotics
How do antibiotics alter the CSF profile and culture? A common question for ID consultants: is an LP really still helpful if they have already received antibiotics?
- Prior administration of antimicrobials before LP can reduce the yield of Gram stain and culture
- Rogers T, Sok K, Erickson T, et al. Impact of Antibiotic Therapy in the Microbiological Yield of Healthcare-Associated Ventriculitis and Meningitis. Open Forum Infect Dis. 2019;6(3):ofz050. Published 2019 Feb 6. doi:10.1093/ofid/ofz050
- Blazer S, Berant M, Alon U. Bacterial meningitis. Effect of antibiotic treatment on cerebrospinal fluid. Am J Clin Pathol. 1983;80(3):386-387. doi:10.1093/ajcp/80.3.386
- …but it has minimal impact on the chemistry and cytology findings
- Rogers T, Sok K, Erickson T, et al. Impact of Antibiotic Therapy in the Microbiological Yield of Healthcare-Associated Ventriculitis and Meningitis. Open Forum Infect Dis. 2019;6(3):ofz050. Published 2019 Feb 6. doi:10.1093/ofid/ofz050
- Kanegaye JT, Soliemanzadeh P, Bradley JS. Lumbar puncture in pediatric bacterial meningitis: defining the time interval for recovery of cerebrospinal fluid pathogens after parenteral antibiotic pretreatment [published correction appears in Pediatrics 2002 Sep;110(3):651]. Pediatrics. 2001;108(5):1169-1174.
- Geiseler PJ, Nelson KE, Levin S, Reddi KT, Moses VK. Community-acquired purulent meningitis: a review of 1,316 cases during the antibiotic era, 1954-1976. Rev Infect Dis. 1980;2(5):725-745. doi:10.1093/clinids/2.5.725
- Pathogens can still be cultured from the CSF in most patients up to several hours after administration of antibiotics. In this study, they found sterilization of meningococcus within 2 hrs and beginnings of sterilization of pneumococcus by 4 hrs of therapy
- So getting that LP is still valuable for decision-making, as you expect that the CSF analysis derangements (and Gram stain) would be suggestive of bacterial meningitis even after administration of antibiotics!
When do you administer steroids in suspected bacterial meningitis?
- It is recommended to administer dexamethasone as part of empiric therapy for adults with suspected bacterial meningitis with unknown pathogen
- IV administration of glucocorticoids (usually dexamethasone) have been associated with reduced hearing loss, neurologic complications, and mortality in patients with S.pneumoniae meningitis
- Adjunctive dexamethasone should be given shortly before or at the same time as first dose of antibiotics when indicated
- Continue if the CSF Gram stain and/or CSF or blood cultures grow S.pneumoniae
- The efficacy of dex in adults with bacterial meningitis was evaluated in this randomized trial from Europe: de Gans J, van de Beek D; European Dexamethasone in Adulthood Bacterial Meningitis Study Investigators. Dexamethasone in adults with bacterial meningitis. N Engl J Med. 2002;347(20):1549-1556. doi:10.1056/NEJMoa021334
- A follow-up study of the European Dexamethasone Study: Weisfelt M, Hoogman M, van de Beek D, de Gans J, Dreschler WA, Schmand BA. Dexamethasone and long-term outcome in adults with bacterial meningitis. Ann Neurol. 2006;60(4):456-468. doi:10.1002/ana.20944
- Additional resources:
- Brouwer MC, McIntyre P, Prasad K, van de Beek D. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst Rev. 2015;2015(9):CD004405. Published 2015 Sep 12. doi:10.1002/14651858.CD004405.pub5
- van de Beek D, de Gans J, McIntyre P, Prasad K. Steroids in adults with acute bacterial meningitis: a systematic review. Lancet Infect Dis. 2004;4(3):139-143. doi:10.1016/S1473-3099(04)00937-5
- van de Beek D, Farrar JJ, de Gans J, et al. Adjunctive dexamethasone in bacterial meningitis: a meta-analysis of individual patient data. Lancet Neurol. 2010;9(3):254-263. doi:10.1016/S1474-4422(10)70023-5
Infographics
Goal
Listeners will be able to understand the initial management of suspected bacterial meningitis.
Learning Objectives
After listening to this episode, listeners will be able to:
- Discuss the initial testing recommendations for CSF analysis in a patient with suspected meningitis
- Formulate an empiric antibiotic regimen for a patient with suspected bacterial meningitis
- Describe strategies of a clinical teacher that will probe and refine clinical reasoning discussions on ID rounds
Disclosures
Our guests (Katie Sharma, Amalia Aldredge, Varun Phadke) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Aldredge, A., Phadke, V., Sharma, K., Dong, S. “#67: Brain Training”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/dd1d75e9-a8e3-445f-80ff-459cd38702e4