Credits
Host(s): Sara Dong, Jeff Larnard
Guest: Wendy Stead
Writing: Sara Dong, Jeff Larnard
Producing/Editing/Cover Art/Infographics: Sara Dong
Our Guests
Guest Consultant
Wendy Stead, MD

Dr. Stead is the program director of the Beth Israel Deaconess Medical Center (BIDMC) Infectious Diseases Fellowship and an Assistant Professor of Medicine at Harvard Medical School. Dr. Stead completed her Internal Medicine residency and ID fellowship at BIDMC and then joined the BIDMC faculty with a joint appointment in the Divisions of Infectious Diseases and General Medicine and Primary Care in 2003. She also completed a Rabkin Fellowship in Medical Education in 2010. She dedicates herself to patient care, medical education, and curriculum development work at the residency and fellowship levels, winning many awards for teaching, mentorship, and humanistic care. Her active research interests include examining the effects of interdisciplinary education strategies on collaboration between specialty services, communication skills in patients with opioid use disorders, trainee wellness, and gender bias in academic medicine. She also loves narrative medicine and writing stories about her inspiring patients (check out a Piece of her mind here, here, and here or her poetry here)
Guest Co-Host
Jeff Larnard, MD

For better or worse, I am very Massachusetts. I grew up in Amesbury, MA and went to Umass Amherst to study nutrition before going on to Umass Medical School. I had a brief stint in NYC for Internal Medicine residency at Columbia before coming back to Boston to be an Infectious Disease fellow at Beth Israel Deaconess (BIDMC).
My interests include medical education, antimicrobial stewardship, and getting as many pop culture references as possible into presentations and materials. Outside of medicine I love cooking (though maybe not as much as Sara…), running, and enjoying Tom Brady.
Culture
Wendy’s recommendation: David Sedaris‘ When You Engulfed in Flames, essay “That’s Amore”
Consult Notes
Consult Q
Petechial rash concerning for purpura fulminans, assistance with antibiotics and work-up
One-liner
60 year-old male with history of immune thrombocytopenic purpura, prior splenectomy in setting of bleeding (secondary to ITP), and gallstones s/p cholecystectomy who presented with a rapidly progressive purpuric rash/purpura fulminans, septic shock, and disseminated intravascular coagulation.
Key Points
Capnocytophaga Pearls
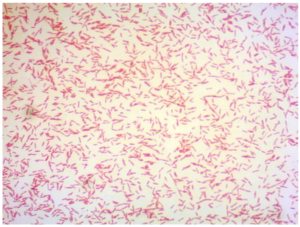
- Micro:
- Gram negative rod with long fusiform shape
- Fastidious! Facultative anaerobe that grows slowly and often needs enriched agar
- Capnophilic (likes increased CO2 concentration)
- Several spp in the genus, but C.animorsus is most common cause of severe disease in humans
- Normal flora in oral cavity of dogs (and cats)
- Pathogenesis of severe disease is not well understood
- Classic clinical scenario: septic shock with fever, disseminated purpuric lesions, disseminated intravascular coagulation (DIC), hypotension, acute renal failure, altered mental status → can evolve to purpura fulminans or gangrene
- Risk factors for disease: contact with dog (bites, scratches, etc), immunocompromised host, asplenia, cirrhosis, history of heavy alcohol use
- Treatment: beta-lactam + beta-lactamase combination (e.g. Piperacillin-Tazobactam) or carbapenem pending susceptibility testing
- Rate of beta-lactam resistance is not clear, but appears to be rising
- Fluoroquinolones, aminoglycosides, macrolides have variable susceptibility
- Butler T. Capnocytophaga canimorsus: an emerging cause of sepsis, meningitis, and post-splenectomy infection after dog bites. Eur J Clin Microbiol Infect Dis. 2015;34(7):1271-1280. doi:10.1007/s10096-015-2360-7
- Roscoe DL, Zemcov SJ, Thornber D, Wise R, Clarke AM. Antimicrobial susceptibilities and beta-lactamase characterization of Capnocytophaga species. Antimicrob Agents Chemother. 1992;36(10):2197-2200. doi:10.1128/aac.36.10.2197
Fever in a patient with impaired splenic function (asplenia or hyposplenia) is a medical emergency. The list of causes of asplenia/hyposplenia is long and includes:
- Iatrogenic (e.g. surgical splenectomy)
- Hematologic disease or malignancy
- Vascular thrombosis
- Autoimmune disorders
- Infiltrative disease (amyloidosis, sarcoidosis)
- Gastrointestinal/hepatic disease
- Congenital syndromes
Is there a difference in risk in someone who has anatomic asplenia vs functional or partial hyposplenism? Is there a ballpark number you can counsel your patients with when thinking about the relative risk when asplenic vs. their normal spleen-ed neighbor?
- Risk is not equal among patients with functional hyposplenism, so there can be some degree of individualization → but most physicians likely favor treating patients along the spectrum of hyposplenia to asplenia conservatively and in the same way
- Relative risk of infection, sepsis, sepsis-related mortality is about ~2-3x higher in asplenic pts vs general population. This risk is sustained over lifetime and pts are predisposed to subsequent episodes
- Here is a cohort study of >8,000 splenectomized patients (American veterans) over 27 years. Asplenic pts had increased risk of hospitalization for pneumonia, meningitis, sepsis, and sepsis related mortality. Observed risks were increased even 10 years out.
- Here is a prospective multicenter cohort study of overwhelming post-splenectomy infection from Clinical Infectious Diseases
- Here is a review of 1648 splenectomized patients in Scotland. The overall rate of first severe infection was 7 in 100 person years (95% CI 6.3-7.78), and the rates of infection were highest in those in their 60-70s. 50-80% of severe infection or death occurred within 1-3 years after splenectomy. Antibiotic prophylaxis likely offered most benefits in the first 3 years after splenectomy or the first 6 months after occurrence of first severe infection
- Here is a more recent retrospective cohort study reviewing data from Victorian Spleen Registry in Australia on overwhelming post-splenectomy sepsis.
Key pathogens to consider with asplenia!
- Encapsulated bacteria
- **S.pneumoniae, estimated to account for 40-60% of severe cases but has declined with vaccination
- H.influenzae type b, which has also declined with vaccination
- Neisseria meningitidis: less common (prob <3%)
- Capnocytophaga spp: C.animorsus, C.cynodegmi; dog bites
- Estimated 12% of reported cases in asplenic pts
- Bloodborne parasites
- Malaria
- Babesiosis
- Bordetella holmesii: respiratory pathogen that causes pertussis-like sxs in immunocompetent pts but knowledge is limited
How to counsel a patient about asplenia (e.g. pre-splenectomy outpatient visit)
Educating patients and families about the lifelong risk of infection with asplenia is critical. Your counseling should emphasize strategies to minimize risk. The keys to remember are:
- Increased lifelong risk of severe infection
- Importance of vaccination (see details below)
- Use of emergency antibiotic prophylaxis
- When to seek medical care
- Patients should seek medical care with fever or evidence of systemic infection
- Would also counsel on need to seek immediate care for animal bites or tick bites in endemic areas
- Lastly, patients should be evaluated for pre-travel counseling when needed, especially if expected to travel to malaria endemic region
What are the key vaccinations for patients with asplenia? Vaccines focus on the organisms of concern with asplenia! You can use “2-2-1” to remember: two Strep pneumoniae, two N.meningitidis, one HiB:
- PCV13, followed by PPSV23 8 wks later
- HiB
- MenACWY and MenB series
- Seasonal influenza
- As always, would also recommend age-appropriate vaccinations
Ideally would administer vaccines as soon as possible. If the patient is planned for surgery, would try to avoid the 14 days before and after operation due to concern for inadequate antibody response to vaccination in that timeframe.
Here is a paper summarizing vaccination recommendations:
Check out the CDC Table 2. Recommended Adult Immunization Schedule by Medical Condition and Other Indications, United States, also reproduced below:
What antibiotic prophylaxis should you recommend?
- Antibiotic prophylaxis can reduce risk of infection and poor outcomes in patients with asplenia
- All patients should receive empiric emergency antibiotics, often known as “pill in pocket”. These are on hand for development of fever or other signs of systemic infection.
- Choice of antibiotic = Amoxicillin-Clavulanate in adults and children
- Alternate options for penicillin allergic: fluoroquinolones (Levofloxacin or Moxifloxacin), cefdinir
- Recommendations for oral daily antibiotic prophylaxis are variable.
- Some may recommend daily prophylaxis in patients considered high risk, such as: children under the age of 5, immunocompromised hosts, history of severe infection (especially in first 6 months), and the first year post-splenectomy
- Data is limited in most situations though – as studies of effectiveness of prophylactic antibiotics are mostly limited to children with sickle cell disease. Here is a review that looked at the trials comparing prophylactic antibiotics to prevent pneumococcal infection in children with sickle cell disease.
- Rankine-Mullings AE, Owusu-Ofori S. Prophylactic antibiotics for preventing pneumococcal infection in children with sickle cell disease. Cochrane Database Syst Rev. 2017;10(10):CD003427. Published 2017 Oct 10. doi:10.1002/14651858.CD003427.pub4
- Here is the commonly referenced randomized trial from 1986 (PROPS) — placebo controlled trial of oral penicillin V 125mg twice daily in children 3-36 months old with sickle cell disease demonstrated 84% reduction in pneumococcal septicemia: Gaston MH, Verter JI, Woods G, et al. Prophylaxis with oral penicillin in children with sickle cell anemia. A randomized trial. N Engl J Med. 1986;314(25):1593-1599. doi:10.1056/NEJM198606193142501
- This was followed by PROPS II in 1995: Falletta JM, Woods GM, Verter JI, et al. Discontinuing penicillin prophylaxis in children with sickle cell anemia. Prophylactic Penicillin Study II. J Pediatr. 1995;127(5):685-690. doi:10.1016/s0022-3476(95)70154-0
- In addition to the fact that data are lacking on effectiveness and appropriate duration of prophylactic daily antibiotics in other settings, it is also unclear how this has evolved in context of routine use of PCV13 and pneumococcal antimicrobial resistance (the risk reduction might not be this large today even in the populations previously studied).
- What does the Red Book say? Red Book recommends daily antimicrobial prophylaxis for infants with sickle cell anemia as soon as diagnosed, preferably by 2 months of age. Less agreement exists exists in other settings but generally recommended if: younger than 5 years old, for at least 1 year after splenectomy at any age. Age to stop prophylaxis could be 5 years old (based on prior study), but some experts may continue prophylaxis in “particularly high risk patients”
- Can consider prophylaxis prior to procedures with increased risk of encapsulated organism infections, such as sinus and respiratory tract, in some situations
Other miscellaneous mentions and notes
- Like textbook references? Check out these chapters:
- Mandell, Principles and Practice of ID, 8th Ed.: Chapter 316: Infections in Asplenic Patients
- Long, Principles and Practice of Pediatric ID, 5th Ed.: Chapter 106: Infectious Complications in Special Hosts, Asplenia and Polysplenia
- You can look at the website for Spleen Australia for some great resources for patient education as well as clinicians. Check out the Spleen Australia guidelines for prevention for sepsis here:
- Here are guidelines from British Committee for Standards in Haematology, last updated 2011:
- A NEJM Clinical Practice article on “Care of the Asplenic Patient”: Rubin LG, Schaffner W. Clinical practice. Care of the asplenic patient. N Engl J Med. 2014;371(4):349-356. doi:10.1056/NEJMcp1314291
- In case you need more humor (and dancing spleens) in your life: What Does the Spleen Do? Featuring Harvard Medical School students
- If you’d like to read a little more about cirrhosis-associated immune dysfunction:
Goal
Listeners will be able to form comprehensive differential diagnosis for overwhelming post-splenectomy sepsis
Learning Objectives
After listening to this episode, listeners will be able to:
- Identify Capnocytophaga as cause of sepsis and purpura fulminans in asplenic patients
- Recognize fever in a patient with impaired splenic function is a medial emergency
- Identify key pathogens that lead to infection in asplenic or hyposplenic individuals
- List the key vaccinations indicated for patients with asplenia
- Describe the appropriate patient education to provide when counseling patients with asplenia
Disclosures
Our guest (Dr. Wendy Stead) as well as the Febrile Podcast and hosts report no relevant financial disclosures.
Citation
Stead, W., Dong, S., Larnard, J. “#1: You’ve got some ex-spleen-in’ to do”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/9accbc32-9994-4592-b2cc-55c0260dbb64