Credits
Host(s), Writing: Jordan Mah, Sara Dong
Guest: Ilan Schwartz
Producing/Editing/Cover Art: Sara Dong
Infographics: Marcela Santana, Sara Dong
Our Guests
Ilan Schwartz, MD, PhD

Ilan Schwartz is an Assistant Professor at the University of Alberta. He completed his Infectious Diseases residency at the University of Manitoba, followed by a PhD from the University of Antwerp in Belgium, where he studied clinical and environmental aspects of a novel fungus described as Emergomyces africanus in South Africa. Following this, he undertook a research fellowship at the San Antonio Center for Medical Mycology in Texas. He is a clinician researcher with interest in mycology and immunocompromised hosts. He is a Fellow of the European Confederation of Medical Mycology, and a co-author of the ECMM global guidelines for the diagnosis and management of the endemic mycoses.
Jordan Mah, MD

Dr. Jordan Mah is an ID fellow at the University of Calgary. He completed his MD at the University of Toronto, followed by Internal Medicine at McGill University. He has an interest in tropical medicine, immigrant health, and tuberculosis
Marcela Araújo de Oliveira Santana

I am a medical student at Federal University of Uberlândia, completing my final year (6th year). I was born and raised in a small village in Minas Gerais, Brazil. I am hoping to be an internal medicine resident soon with the intent of specializing in infectious diseases! My interests are medical education, infectious diseases (especially tropical diseases), and rural health! I love reading (I am a big fan of dystopias), cooking, and playing board games with my friends.
Culture
Ilan’s favorite is traveling with his family!
Consult Notes
Consult Q
50 year old female with fever, cough, pancytopenia, and an abnormal chest CT
Case Summary
50 year old female who presented with fever, cough, and weight loss who was initially diagnosed with presumed tuberculosis but ultimately found to have disseminated histoplasmosis. Her course was later complicated by immune reconstitution inflammatory syndrome
Key Points
Jump to:
"Fungi are the interface organisms between life and death"
Paul Stamets, Mycelium Running Tweet
Ilan gave a great differential diagnosis based on his problem representation in this case and episode. Here is a general summary of the broad differential diagnosis of fever with miliary (diffuse micronodular) infiltrates on pulmonary imaging – it’s not just TB!! This is a long list with several items that are less likely, so would keep TB, fungal disease, and malignancy as top of the list in majority of cases!
- Tuberculosis is top of the list!!!!
- The name “miliary TB” came from the similar appearance of millet seeds to lesions seen in gross pathology and later imaging. Millets are small grains (average diameter <2mm)
- Fungal
- Histoplasmosis, coccidioidomycosis, blastomycosis are the most described
- Others: paracoccidioidomycosis, cryptococcosis, talaromycosis, emergomycosis
- Pneumocystis jiroveci pneumonia
- Neoplastic disease
- Lymphoma
- Lymphangitic spread of carcinoma
- Mesothelioma
- Nontuberculous mycobacteria
- Bacterial
- Legionella micdadei
- Nocardiosis
- Staph aureus, H.influenza, or pyogenic bacteria
- Psittacosis
- Tularemia
- Bartonellosis
- Brucellosis
- Melioidosis
- Rhodococcus
- Viral
- Varicella
- Cytomegalovirus
- Influenza
- Measles
- Parasitic
- Toxoplasmosis
- Strongyloidiasis
- Schistosomiasis
- Paragonomiasis
- Others
- Sarcoidosis
- Amyloidosis
- Hypersensitivity pneumonitis
- Pneumoconioses (silicosis, coal workers pneumoconiosis)
- Foreign body-induced vasculitis related to injection drug use
- E-cig and vaping associated hypersensitivity reactions
- Pulmonary alveolar proteinosis
Here is an example case from Annals of ATS that highlights the differential diagnosis as well: Kimmig L, Bueno J. Miliary Nodules: Not Always Tuberculosis. Ann Am Thorac Soc. 2017;14(12):1858-1860. doi:10.1513/AnnalsATS.201706-436CC
An overview of histoplasmosis below!
Epidemiology & Mycology
- Histoplasma is an endemic dimorphic fungi in the family Ascomycetes
- Dimorphic means Histoplasma exists as mold (mycelial) form in the environment and then converts to yeast form at body temperature
- Previously thought to only have 2 species (H.capsulatum, H.duboisii), but we now know the genetic diversity is vast with at least 7 different species in the complex
- The mycelial phase reveals two types of conidia:
- Macroconidia: large, ovoid, 8-15µm, protrusions on surface (tuberculate)
- Microconidia: small, round, 2-5 µm – thought to be infective phase due to small size that can lodge in bronchioles and alveoli
- Worldwide distribution (has been noted on every continent except Antarctica)
- Classically endemic to North America, notably described in the Ohio and Mississippi River valleys
- Also endemic in areas of Central and South America, Asia, and Africa
- Bahr NC, Antinori S, Wheat LJ, Sarosi GA. Histoplasmosis infections worldwide: thinking outside of the Ohio River valley. Curr Trop Med Rep. 2015;2(2):70-80. doi:10.1007/s40475-015-0044-0
- Ashraf N, Kubat RC, Poplin V, et al. Re-drawing the Maps for Endemic Mycoses. Mycopathologia. 2020;185(5):843-865. doi:10.1007/s11046-020-00431-2
- Risk factors are generally related to exposure to bird or bat guano + soil:
- Spelunking (cave exploration)
- Exposure to birds, bird roosts, chicken coops, farm buildings with large accumulation of bird droppings
- Soil exposure such as those engaged in agriculture
- Excavation or construction with disruption of soil, including outdoor construction and rehabilitation of buildings inhabited by birds or bats
- Notes:
- Many patients will not recall a specific exposure
- Human-to-human transmission via pulmonary route has not been reported
- In rare occasions Histoplasma has been transmitted via infected organ transplant
- Limaye AP, Connolly PA, Sagar M, et al. Transmission of Histoplasma capsulatum by organ transplantation. N Engl J Med. 2000;343(16):1163-1166. doi:10.1056/NEJM200010193431605
- Kauffman CA, Miceli MH. Histoplasmosis and Blastomycosis in Solid Organ Transplant Recipients. J Fungi (Basel). 2015;1(2):94-106. Published 2015 Jun 30. doi:10.3390/jof1020094
- Nel JS, Bartelt LA, van Duin D, Lachiewicz AM. Endemic Mycoses in Solid Organ Transplant Recipients. Infect Dis Clin North Am. 2018;32(3):667-685. doi:10.1016/j.idc.2018.04.007
- Spores are aerosolized after contaminated soil is disturbed and circulate in the air
- After inhaled, the microconidia undergo a temperature-dependent transformation into yeast cells
- Engulfed by macrophages (which can ingest but not kill the fungi), which can disseminate through body
Clinical forms of histoplasmosis
- *Majority of infections will be asymptomatic or mild and nonprogressive in healthy hosts*
- Acute symptomatic pulmonary histoplasmosis
- Typical incubation is between 7-21 days (commonly ~2 wks)
- Influenza-like illness with fever, cough, chest pain, headache, malaise, fatigue
- **Might be indistinguishable from community acquired pneumonia or viral upper respiratory syndrome
- Focal patchy or nodular infiltrates on chest imaging. A clue may be mediastinal or hilar lymphadenopathy on imaging
- Rheumatologic manifestations may accompany acute pulmonary infection: arthralgias, erythema nodosum or multiforme
- Pericarditis may also occur rarely. Organisms rarely found in tissue or pericardial fluid, so thought to not be direct invasion but rather granulomatous inflammatory response (in mediastinal lymph nodes adjacent to pericardium)
- Severity is thought to correlate with higher spore exposure
- Complications or sequelae:
- Acute re-infection can occur if re-exposed to large inoculum
- Persistent mediastinal granuloma may occur with massive enlargement of mediastinal lymph nodes from exuberant granulomatous inflammation. Nodes can impinge on major local airways, pulmonary vessels, or esophagus leading to post-obstructive pneumonia, bronchiectasis, or SVC syndrome.
- Fibrosing mediastinitis: after abnormal host inflammatory response, can develop calcification and fibrosis. Might not be able to identify prior acute episode of histoplasmosis. No effective treatment with steroids or antifungals
- Histoplasmoma: mass lesion that resembles fibroma
- Chronic pulmonary histoplasmosis
- Can be due to initial / primary infection or reactivation later
- Symptoms >6 weeks duration (low grade fever, cough, dyspnea, weight loss) and evidence of progressive pulmonary infiltrates or cavities
- Symptoms may resemble pulmonary TB or lung cancer with fevers, weight loss, hemoptysis
- Also often characterized by fibrotic apical infiltrates with or without cavitation. Areas can enlarge and may results in formation of bronchopleural fistulae in rare cases
- Often described in men over the age of 50 with chronic lung disease
- Progressive disseminated histoplasmosis
- More common in immunocompromised hosts such as those with advanced HIV/AIDS, solid organ or hematopoietic stem cell transplant recipients, TNF-alpha blockade, elderly, or cellular immunodeficiency
- Fevers, respiratory symptoms, weight loss → spread through reticuloendothelial system can lead to lymphadenopathy, hepatosplenomegaly, bone marrow infiltration
- Possible presentations:
- Adrenal insufficiency
- Oral ulcers that may be painful and with heaped up borders resembling cancer
- GI: colonic mass lesions, colitis with ulcerations
- Cutaneous dissemination: typically nodules, papules, plaques, or ulcers
- Ocular: uveitis or panophthlamitis
- CNS involvement
- Endocarditis
- Labs can demonstrate pancytopenia, transaminitis, elevated alk phos
- Presentation can often be rapidly progressive, but there are some patients who might have subacute or chronic wasting type illness
- High case fatality rate
- Need high index of suspicion and often misdiagnosed as disseminated TB
Diagnostics
- Histopathology:
- Yeast-phase organisms are ovoid, 2-4 microns, and have narrow based budding
- Can appear similar to C.glabrata, C.neoformans, P.jirovecii
- Other findings: granulomas (most cases), lymphohistiocytic or mononuclear cell infiltrates
- Yeast-phase organisms are ovoid, 2-4 microns, and have narrow based budding
- Fungal culture
- Most useful in chronic pulmonary histoplasmosis and less useful in localized or acute disease
- Incidence of positive cultures varies and often is related to number of specimens, burden of infection, and culture source. Multiple sputum or BAL cultures are more likely to produce yield
- Yield for blood cultures are higher if lysis centrifugation technique is used
- May not grow in culture for 6 wks
- Antigen: Histoplasma antigen detection EIA
- Available for urine, blood, or BAL
- In prior study, urinary antigen was been detected in 83% patients with acute pulmonary histoplasma and 92% of patients with disseminated disease. There is higher sensitivity when obtaining both urine and serum (100% in 31 cases of disseminated histo)
- A look at Ag use in BAL samples: Hage CA, Davis TE, Fuller D, et al. Diagnosis of histoplasmosis by antigen detection in BAL fluid. Chest. 2010;137(3):623-628. doi:10.1378/chest.09-1702
- Watch for cross-reactivity: blastomycosis, coccidioidomycosis, talaromycosis, paracoccidioidomycosis
- Serology
- Complement fixation
- Slightly more sensitive but less specific than immunodiffusion
- Titer 1:32 or higher are suggestive of acute infection
- Positive results can also represent persistent antibody response from prior episode of histoplasmosis or infection with other fungi as well as certain granulomatous diseases
- Immunodiffusion
- Greater specificity
- Reported as M or H precipitins (bands)
- Most will develop an M band
- H band detected in <20% cases and most often in those with disseminated or severe disease
- M band is positive sooner and persists longer (so isolated M band could be very early disease or late disease)
- Enzyme immunoassay (EIA) in some labs
- Complement fixation
- Role of PCR less clear. Some results from study in 2015: Muraosa Y, Toyotome T, Yahiro M, Watanabe A, Shikanai-Yasuda MA, Kamei K. Detection of Histoplasma capsulatum from clinical specimens by cycling probe-based real-time PCR and nested real-time PCR. Med Mycol. 2016;54(4):433-438. doi:10.1093/mmy/myv106
Treatment
Wheat LJ, Freifeld AG, Kleiman MB, et al. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45(7):807-825. doi:10.1086/521259 (New IDSA guidelines are in the works)
See a summary chart compiled below:
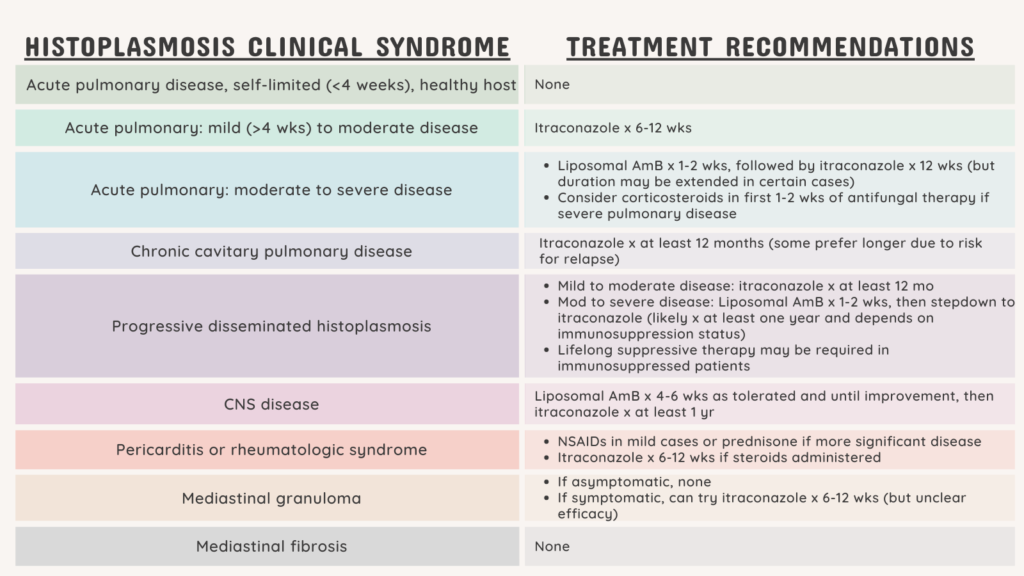
- Generally will have induction phase with liposomal amphotericin B, usually 1-2 weeks depending on clinical response → then transition to itraconazole
- Duration of treatment depends on host and disease response, but generally at least 12 mo if immunocompromised host. Ultimate decision will be guided by status of their immunocompromising condition
- Clearance of antigenemia is a useful tool examining clinical response, although some patients might not have Ag test positive initially to follow.
- Notes on itraconazole:
- Itraconazole can be tricky.
- Capsules need gastric acid for enhanced bioavailability:
- Take with food
- Acidic beverages like regular cola or orange juice can increase gastric acidity and absorption
- Capsules are well tolerated but the exposures are unpredictable, so need to follow levels.
- A liquid formulation is available and overcomes poor capsule absorption
- Must be given on empty stomach
- But it causes more GI upset and diarrhea, which is often difficult for patients
- There is also a newer formulation of itraconazole with enhanced bioavailability in the US, but may not be easily available in most places
- Watch for drug-drug interactions with itraconazole (and other azoles): concomitant use of antacids, H2 blockers, or PPIs may cause treatment failure
- Negative inotropy and CHF exacerbations can be seen with itraconazole
- Other notes:
- Alternatives include: posaconazole, voriconazole, isavuconazole – although no clinical trials have compared these different azoles for histoplasmosis
- Posaconazole in particular has been shown effective as salvage therapy
- Voriconazole is probably less active than itra and posa, but has been used in some
- Isavuconazole is active but limited clinical experience
- Wheat LJ, Connolly P, Smedema M, et al. Activity of newer triazoles against Histoplasma capsulatum from patients with AIDS who failed fluconazole. J Antimicrob Chemother. 2006;57(6):1235-1239. doi:10.1093/jac/dkl133
- Thompson GR 3rd, Rendon A, Ribeiro Dos Santos R, et al. Isavuconazole Treatment of Cryptococcosis and Dimorphic Mycoses. Clin Infect Dis. 2016;63(3):356-362. doi:10.1093/cid/ciw305
- Fluconazole and echinocandins have poor activity
- Wheat J, MaWhinney S, Hafner R, et al. Treatment of histoplasmosis with fluconazole in patients with acquired immunodeficiency syndrome. National Institute of Allergy and Infectious Diseases Acquired Immunodeficiency Syndrome Clinical Trials Group and Mycoses Study Group. Am J Med. 1997;103(3):223-232. doi:10.1016/s0002-9343(97)00151-4
- McKinsey DS, Kauffman CA, Pappas PG, et al. Fluconazole therapy for histoplasmosis. The National Institute of Allergy and Infectious Diseases Mycoses Study Group. Clin Infect Dis. 1996;23(5):996-1001. doi:10.1093/clinids/23.5.996
- Wheat LJ, Connolly P, Haddad N, Le Monte A, Brizendine E, Hafner R. Antigen clearance during treatment of disseminated histoplasmosis with itraconazole versus fluconazole in patients with AIDS. Antimicrob Agents Chemother. 2002;46(1):248-250. doi:10.1128/AAC.46.1.248-250.2002
- Hage CA, Connolly P, Horan D, et al. Investigation of the efficacy of micafungin in the treatment of histoplasmosis using two North American strains of Histoplasma capsulatum. Antimicrob Agents Chemother. 2011;55(9):4447-4450. doi:10.1128/AAC.01681-10
- Alternatives include: posaconazole, voriconazole, isavuconazole – although no clinical trials have compared these different azoles for histoplasmosis
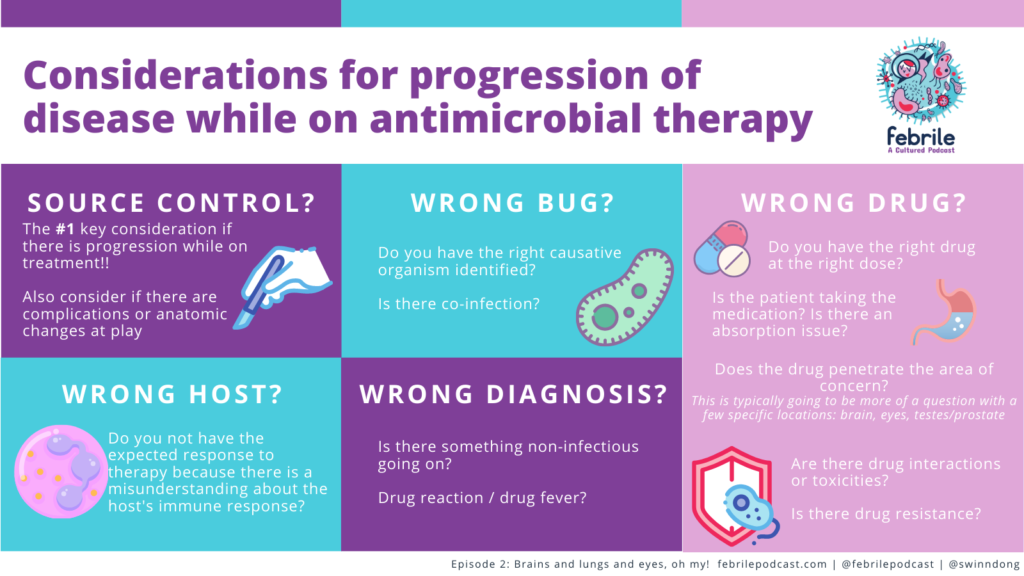
The end of the episode covered an approach to a patient who is not responding as expected to therapy. Some possibilities include the items below and are summarized in the graphic. In this case:
- Go back to the diagnosis!
- Is this a progressive infection with the same bug? A new co-infection?
- Is there a different explanation or secondary process (autoimmune process?)
- Is there an issue with the drug? Can it get to the site of infection? Absorbed? Interactions?
- Do you need to consider an underlying immunodeficiency?
- An example in this case was IFN-gamma deficiency which has been described in non-HIV patients from Thailand or Taiwan (we’ve mentioned previously on Febrile, check out a paper here) vs other defects in cellular mediated immunity
- Is this a process driven by inflammation? Don’t forget that immune reconstitution inflammatory syndrome (IRIS) can occur in non-HIV population
Other miscellaneous mentions and notes:
Textbook references
- Mandell, Principles and Practice of ID, 8th Ed., 9th Ed.:
- Chapter 265: Histoplasma capsulatum (Histoplasmosis)
- Comprehensive Review of Infectious Diseases:
- Chapter 2: Mycology
- Chapter 28: The Dimorphic Mycoses
Episode Art & Infographics
Goal
Listeners will be able to describe the epidemiology, diagnosis, and treatment of histoplasmosis.
Learning Objectives
After listening to this episode, listeners will be able to:
- Create a differential diagnosis for miliary pulmonary opacities on imaging
- Compare and contrast available non-culture based diagnostics for histoplasmosis
- Describe the types of immunocompromised hosts most at risk for disseminated progressive histoplasmosis
Disclosures
Our guest (Ilan Schwartz) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Schwartz, I., Mah, J., Dong, S. “#27: Millet Seeds of Destruction”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/47a371e7-83ca-4cf6-804e-4141f1accce5


