Credits
Host: Sara Dong
Guest: Rebecca Kumar
Writing/Producing/Editing/Cover Art/Infographics: Sara Dong
Our Guest
Rebecca Kumar, MD, MS

Dr. Rebecca Kumar is a Transplant ID physician and assistant professor at MedStar Georgetown University Hospital in the Division of Infectious Diseases and Tropical Medicine. She previously completed her internal medicine residency at Medstar Georgetown University Hospital in Washington DC followed by fellowship in infectious diseases at Northwestern University in Chicago.
Consult Notes
Consult Q
assistance in work-up of fever and pain/purulent drainage from driveline exit site
One-liner
70 year old male with CAD s/p CABG and ischemic HFrEF s/p LVAD who presented with fevers with pain and purulence from driveline site. He was found to have deep driveline infection.
Key Points
Jump to:
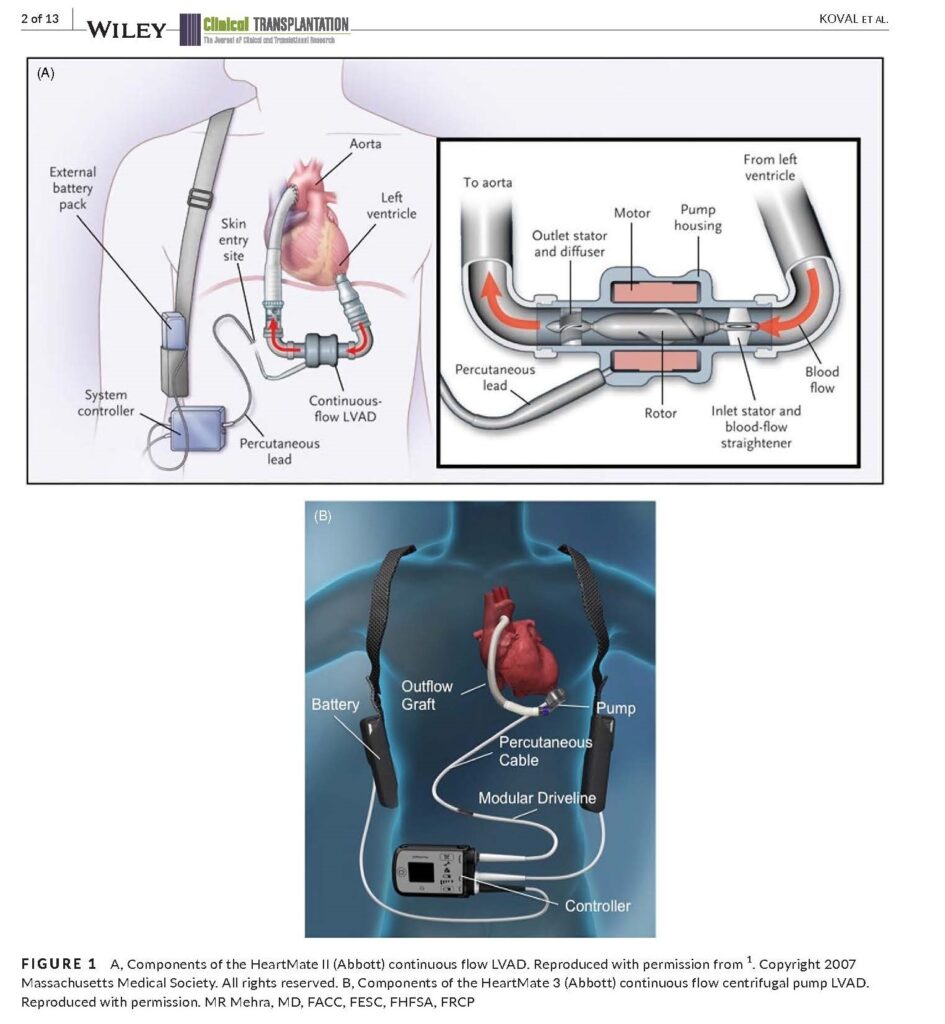
We started this episode with an overview of ventricular assist devices or VADs.
These devices are mechanical pumps that provide circulatory support by augmenting the ability of a failing heart to deliver blood flow in patients with refractory heart failure
- VADs are usually continuous flow, now with a centrifugal pump (sort of like a rotor floating between two magnets)
- The newer pumps tend to last longer with less hemorrhagic and thrombotic complications that were seen in earlier pulsatilla pumps (a look at continuous flow devices from NEJM here)
- Use different speeds to mimic increases/decreases in flow
- Newer VADs are also smaller, implanted directly into the pericardium (previously there were preperitoneal pump pockets), and have smaller caliber drivelines (which are more durable)
- Some possible brands/devices you may hear: HeartMate 2, 3 (Abbott); Heartware HVAD (Medtronic), Jarvik Heart
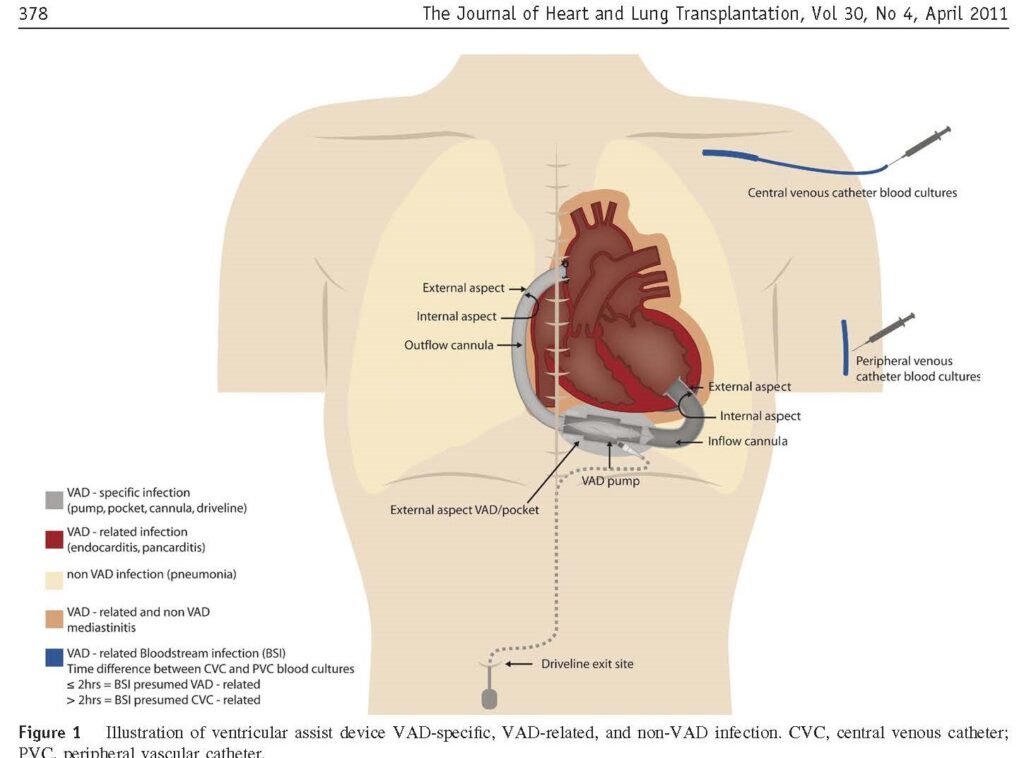
Components of the VAD mentioned on the show
- VADs can be implanted in right or left ventricle, but vast majority are going to be left = LVADs
- Inflow cannula, which connects pumps itself to the heart and allows blood flow
- Outflow cannula, which pumps blood to rest of body
- Driveline runs through the chest and abdomen before exiting in lower abdomen
- Driveline is connected to controller (where cardiologists can adjust) — this is the component that will alarm with outflow obstruction, etc
- Driveline itself has piece of velour near exit site which should stick inside peritoneal space, and this exists to help with granulation tissue formation and seal around driveline.
- When this is pulled out / exposed, it is a great place for bacteria to grow
- Battery pack (external)
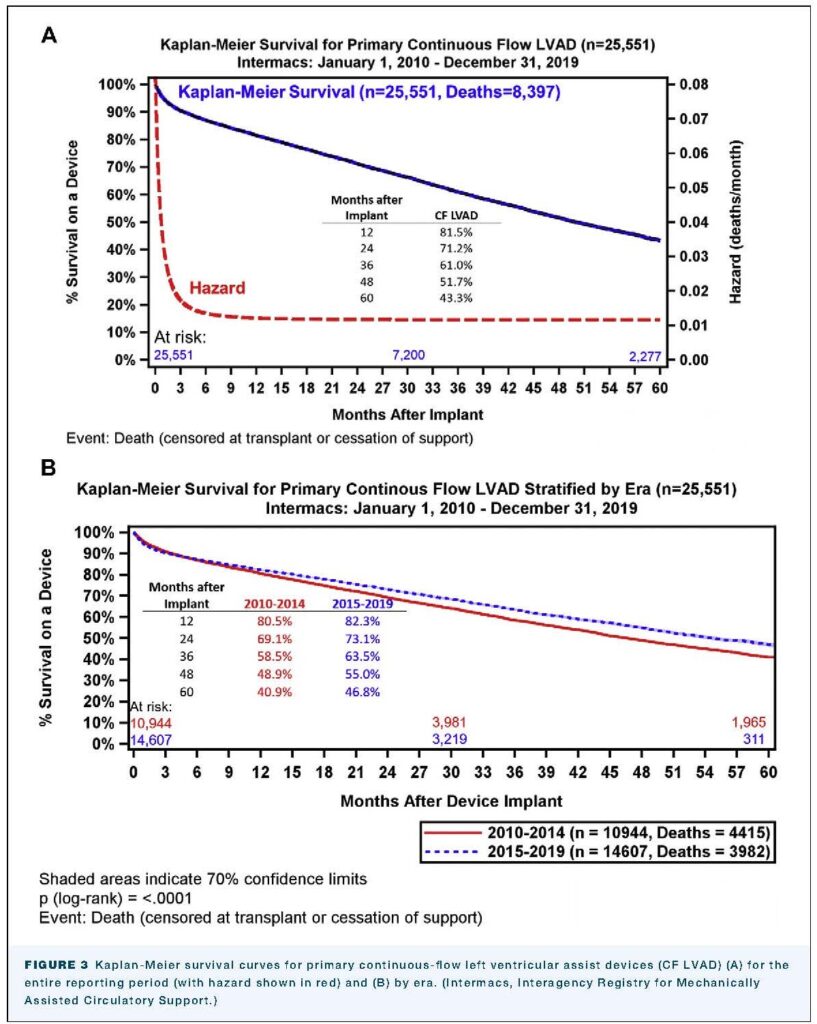
VADs improve survival, functional status, and quality of life. As mentioned on the show, annual reports from the INTERMACS (Interagency Registry for Mechanically Assisted Circulatory Support) database provide information from >20k patients, >180 hospitals, >4000 cases of LVADs
- Survival is now >80% at 1 year, >70% at 2 years, 35% at 5 years
- Average time patients live with device support has increased from 126 to 348 days
- Nearly half are considered destination therapy (DT); 57% are placed in those listed or under evaluation for heart transplant (bridge to transplant)
- Over 40% of heart tx recipients were supported with LVAD prior to transplantation
- Intermacs 2020 annual report: Molina EJ, Shah P, Kiernan MS, et al. The Society of Thoracic Surgeons Intermacs 2020 Annual Report. Ann Thorac Surg. 2021;111(3):778-792. doi:10.1016/j.athoracsur.2020.12.038
- See a few figures below
Infection remains one of the most common complications of VAD therapy and contributes to mortality on the transplant wait list — but many pts with infections are transplanted with excellent outcomes!
Defining VAD Infections
ISHLT (The International Society for Heart & Lung Transplantation) introduced working standard definitions for infection in patients with VADs in 2011. This created the framework of VAD-specific vs. VAD-related vs. non-VAD infections
- Hannan MM, Husain S, Mattner F, et al. Working formulation for the standardization of definitions of infections in patients using ventricular assist devices. J Heart Lung Transplant. 2011;30(4):375-384. doi:10.1016/j.healun.2011.01.717
- Feldman D, Pamboukian SV, Teuteberg JJ, et al. The 2013 International Society for Heart and Lung Transplantation Guidelines for mechanical circulatory support: executive summary. J Heart Lung Transplant. 2013;32(2):157-187. doi:10.1016/j.healun.2012.09.013
As explained by Rebecca and in the document above:
- VAD-specific infections are related to the VAD itself and include:
- Pump pocket and/or cannula infections (the mechanical pump itself or the inflow/outflow cannula has infection)
- Pocket infections (this was more of an issue when the VADs were in preperitoneal pockets)
- Driveline exit site infections, which can be divided into superficial or deep infection (deep implying involvement of musculature and/or soft tissue near driveline site) **most common**
- VAD-related infections include bloodstream infections, infective endocarditis, and mediastinitis. These are infections that are complicated by the presence of a VAD
- Non-VAD infections include items such as UTI, C.difficile, and so on
Here are some references and studies looking at LVAD infections:
- Large international multi-center study of infections of mechanical circulatory support devices: Hannan MM, Xie R, Cowger J, et al. Epidemiology of infection in mechanical circulatory support: A global analysis from the ISHLT Mechanically Assisted Circulatory Support Registry. J Heart Lung Transplant. 2019;38(4):364-373. doi:10.1016/j.healun.2019.01.007
- Siméon S, Flécher E, Revest M, et al. Left ventricular assist device-related infections: a multicentric study. Clin Microbiol Infect. 2017;23(10):748-751. doi:10.1016/j.cmi.2017.03.008
- O’Horo JC, Abu Saleh OM, Stulak JM, Wilhelm MP, Baddour LM, Rizwan Sohail M. Left Ventricular Assist Device Infections: A Systematic Review. ASAIO J. 2018;64(3):287-294. doi:10.1097/MAT.0000000000000684
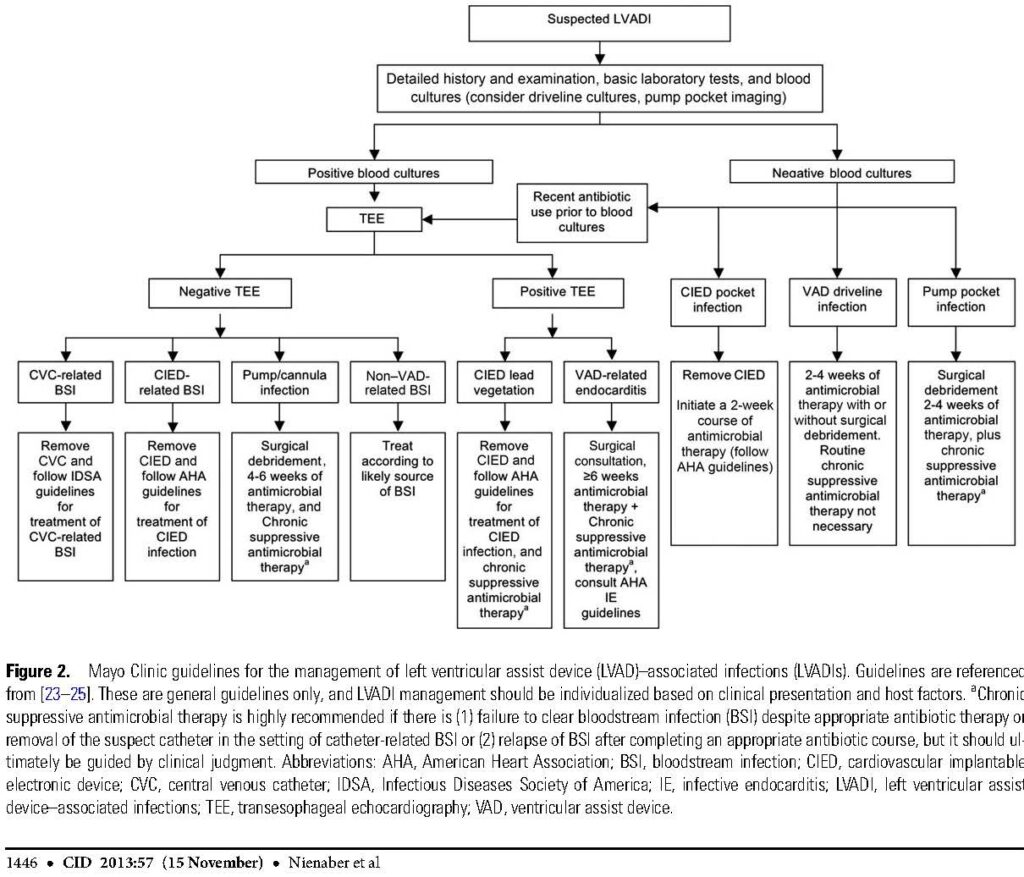
Next we discussed the initial work-up approach when you suspect an LVAD infection
Check out these resources
- AST ID COP guidelines: Koval CE, Stosor V; AST ID Community of Practice. Ventricular assist device-related infections and solid organ transplantation-Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13552. doi:10.1111/ctr.13552
- Nienaber JJ, Kusne S, Riaz T, et al. Clinical manifestations and management of left ventricular assist device-associated infections. Clin Infect Dis. 2013;57(10):1438-1448. doi:10.1093/cid/cit536
In general, the work-up is going to include:
- Blood cultures and other labs
- Evaluation of device, heart valve/CIED involvement (echo)
- Evaluation for local infection (CT or US)
- Check out this flow chart from the Nienaber paper noted above:
Sometimes might want to consider PET scan, here is a case series thinking about this: Tam MC, Patel VN, Weinberg RL, et al. Diagnostic Accuracy of FDG PET/CT in Suspected LVAD Infections: A Case Series, Systematic Review, and Meta-Analysis. JACC Cardiovasc Imaging. 2020;13(5):1191-1202. doi:10.1016/j.jcmg.2019.04.024
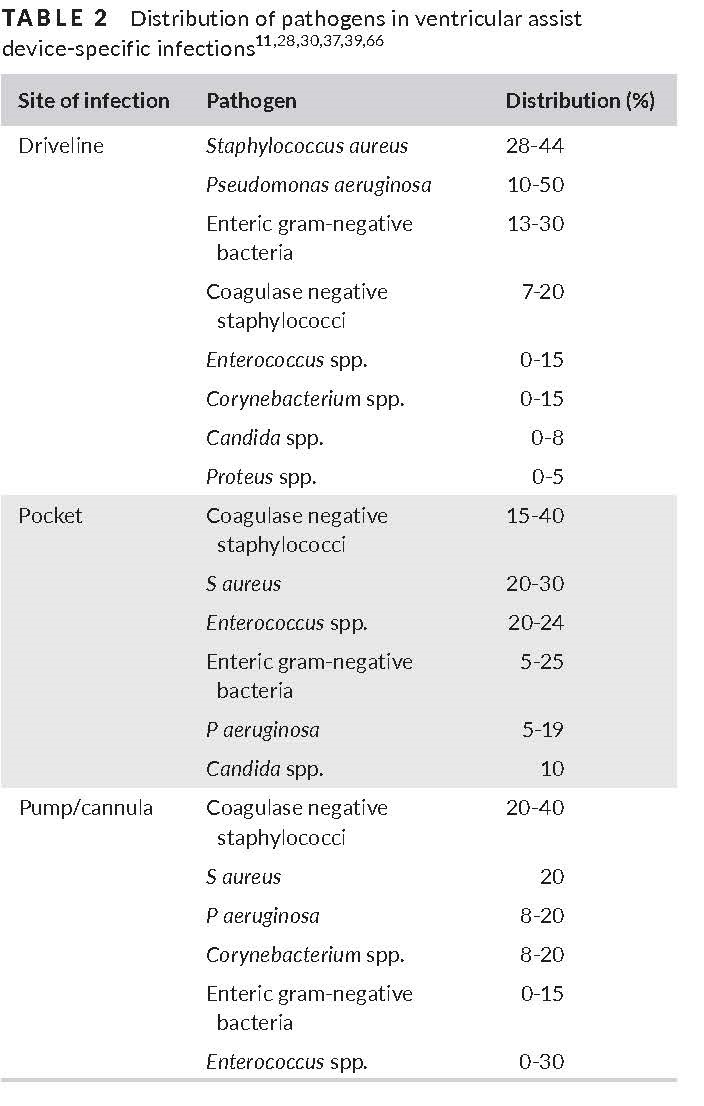
What organisms typically cause VAD infections?
- There is a predominance of Staphylococci (often skin flora, especially in setting of driveline exit site infection)
- Nosocomial gram negative pathogens such as Pseudomonas are a concern as well
- Fungal infections are relatively uncommon
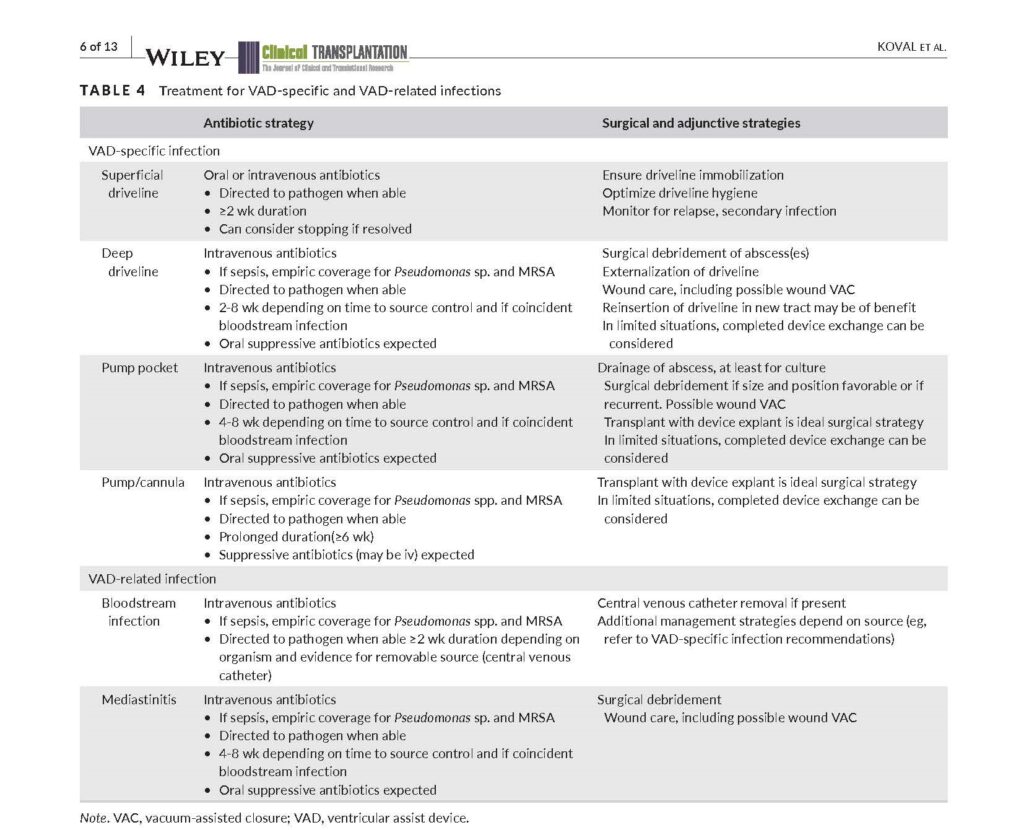
Typical empiric antibiotic coverage for VAD infections would be:
- Based on prior antibiotic exposure, infection history, extent of infection
- Generally will include MRSA coverage as well as additional gram negative (including Pseudomonal) coverage
- +/- anaerobic coverage based on factors noted above
This episode’s case involved a patient with prior superficial driveline infection who had a subsequent deep driveline infection with the same organism. Let’s take a look at general recommendations for management of VAD specific infections in this table
A few final pearls from the episode
- Allergy to chlorhexidine can cause skin breakdown, inflammation, and erythema that mimics superficial driveline infection. There may be certain cases where transition to iodine may improve symptoms
- In cases of suppression antibiotics, it’s important to explain to patient that the ongoing antibiotics are attempting mitigation and not necessarily curing or eradicating the infection
- Driveline trauma (with tugging or pulling on driveline) predisposes to infection. Anchors can be provided to give some slack if there is an accidental pull on the controller/battery
- Here is a nice literature review thinking about risks of LVAD infection: Pavlovic NV, Randell T, Madeira T, Hsu S, Zinoviev R, Abshire M. Risk of left ventricular assist device driveline infection: A systematic literature review. Heart Lung. 2019;48(2):90-104. doi:10.1016/j.hrtlng.2018.11.002
- Bernhardt AM, Schlöglhofer T, Lauenroth V, et al. Prevention and early treatment of driveline infections in ventricular assist device patients – The DESTINE staging proposal and the first standard of care protocol. J Crit Care. 2020;56:106-112. doi:10.1016/j.jcrc.2019.12.014
- Surgical intervention is difficult for VAD infection. In some cases, surgeons may consider moving the driveline exit site or using wound vac for healing with driveline infections
- Make sure you are familiar with your institutions protocol on caring for and examining the driveline exit site. Ideally it would be great to look at the site when possible, but you can also supplement with recent photos as needed.
Other miscellaneous mentions and notes:
- Like textbook references?
- Mandell, Principles and Practice of ID, 8th Ed., 9th Ed.: Cardiovascular Infections > Chapter 84: Infections of nonvalvular cardiovascular devices > Left Ventricular Assist Devices
- Long, Principles and Practice of Pediatric ID, 5th Ed.: Chapter 100: Clinical syndromes of device-associated infections > Infections Associated with Pacemakers and LVADs
- Comprehensive Review of Infectious Diseases
- AAP Red Book
Episode Art & Infographics
Goal
Listeners will be able to identify and evaluate for ventricular assist device infections
Learning Objectives
After listening to this episode, listeners will be able to:
- Describe key components of ventricular assist devices (VADs)
- Define the spectrum of VAD-specific, VAD-related, and non-VAD infections
- Describe the epidemiology and distribution of pathogens in VAD-specific infections
- Discuss the management of VAD-specific infections, especially superficial and deep driveline infections
Disclosures
Our guest (Rebecca Kumar) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Kumar, R., Dong, S. “#30: Shape of My VAD”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/5154e0a3-29fc-4e61-b52f-eef110b32f4e