Credits
Host(s): Jonathan Ryder, Sara Dong
Guest: Nico Cortes-Penfield
Writing: Jonathan Ryder, Nico Cortes-Penfield
Producing/Editing/Cover Art: Sara Dong
Infographics: Jonathan Ryder, Sara Dong
Our Guests
Guest Consultant
Nico Cortes-Penfield, MD
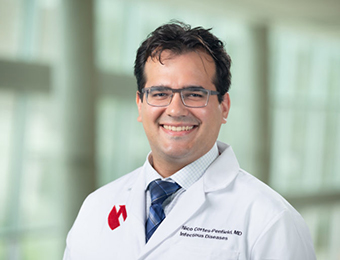
Nico is an assistant professor in the division of infectious diseases at University of Nebraska Medical Center in Omaha, Nebraska. He serves as the medical director of the outpatient parenteral antibiotic therapy program and an associate medical director of antimicrobial stewardship. He did his medical school, residency, and fellowship training at Baylor College of Medicine. His clinical and research interests are in complicated bone and joint infections, as he is part of the core faculty in the orthopedic infectious diseases service line at UNMC.
Guest Co-Host
Jonathan Ryder, MD

Jonathan Ryder, MD is an infectious diseases fellow at University of Nebraska Medical Center in Omaha, NE. He completed his internal medicine residency at Indiana University. His academic interests include medical education, endocarditis, and antimicrobial stewardship. He enjoys podcasts and #IDTwitter. His hobbies include running, reading non-fiction, and NFL football.
Culture
Check out archive.org! It’s a non-profit library with millions of free books, movies, software, music, websites, and more
Consult Notes
Consult Q
Orthopedic surgery is calling about an older male patient with a red, swollen, and painful joint, please evaluate and provide antibiotic recommendations
Case Summary
54 year old male with history of diabetes mellitus type 2, rheumatoid arthritis on infliximab, and recent right total knee arthroplasty for OA who presented with right knee pain and swelling 2 months after his TKA. He was found to have an MRSA PJI and underwent 2-stage exchange. His course was later complicated by wound dehiscence and infection for which he underwent DAIR.
Febrile Survey!

We are conducting a research survey to better understand listener utilization and satisfaction with the Febrile podcast and learning resource. We want to better understand how you use Febrile podcast to teach and learn, but also what we can do to improve for future episodes! The survey is open to anyone who has listened or viewed material from Febrile and is voluntary. This survey takes 5-10 minutes to complete, and responses are completely anonymous. If you have any questions about the survey, you can send me (Sara Dong) an email at swdong@bidmc.harvard.edu. Thank you!
Survey Link: https://hms.az1.qualtrics.com/jfe/form/SV_6o2iYLc1Sq7PMQC
Additional link
Link for registration for IDSA Fellows Peer Mentorship Program: https://docs.google.com/forms/d/e/1FAIpQLSdSBny4BGbo3-LTcv0mBd5IIJ7nHQXvTJhoEY0FAuMO3BrSZA/viewform
Key Points
What are the risk factors for prosthetic joint infection (PJI)?
- In general:
- Knee arthroplasties are both the most likely to become infected and most difficult to treat
- Shoulder arthroplasties are rarely infected and usually do well
- Hips are somewhere in the midline
- Nico divided the risk factors for PJI into 3 main buckets:
- Immunocompromised state (such as RA, DM, CKD, treatment with steroids or TNF alpha inhibitors)
- Things that make surgery or wound healing more difficult (obesity, prior PJI, or revision arthroplasty)
- Disseminated infection (Staph aureus bacteremia, occasionally invasive Strep infection)
- Dental work is frequently misbelieved to be a risk factor for PJI, but prescribing antibiotic prophylaxis before dental procedures for patients with arthroplasties is not evidence-based. Both the ADA and AAOS advise against it.
- Check out the paper mentioned in the podcast below:
- Thornhill MH, Crum A, Rex S, et al. Analysis of Prosthetic Joint Infections Following Invasive Dental Procedures in England. JAMA Netw Open. 2022;5(1):e2142987. Published 2022 Jan 4. doi:10.1001/jamanetworkopen.2021.42987
- An observational study of >9000 patients with PJI in England, where no one gets antibiotic prophylaxis with dental work to prevent PJI → no temporal association between dental procedures and developing PJI
- Check out the paper mentioned in the podcast below:
- Berbari EF, Osmon DR, Lahr B, et al. The Mayo prosthetic joint infection risk score: implication for surgical site infection reporting and risk stratification. Infect Control Hosp Epidemiol. 2012;33(8):774-781. doi:10.1086/666641
How do PJIs present?
- Often presents acutely with pain, stiffness, inability to bear weight on joint over the period of days
- Patients may or may not appear systemically ill, but they often have obvious inflammation at the joint or surgical site
- In less common scenarios, you might see a more indolent presentation of worsening pain and instability over weeks to months (feeling like the leg will give out)
- Patients with subacute onset often do not have fever or leukocytosis, and their physical exam findings may be more subtle
- That said, a few items that should cause suspicion: sinus tracts (a giveaway!), delayed wound healing, ongoing drainage after surgery
Are there available PJI diagnostic criteria?
- The standard diagnostic criteria for PJI are 2018 MSIS criteria. As Nico discussed, these can be used clinically but can also think of these as consensus definition for research
- Parvizi J, Tan TL, Goswami K, et al. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J Arthroplasty. 2018;33(5):1309-1314.e2. doi:10.1016/j.arth.2018.02.078
- Nico pointed out the two major criteria that confirm PJI:
- Presence of sinus tract that communicates with hardware
- Multiple joint cultures (either synovial fluid or tissue) growing the same organism
- If you have either of these, case closed!
- There are also minor criteria worth 1-3 points each, with at least 2 points indicating possible PJI and at least 6 points indicating definite PJI. These include:
- Elevated serum CRP, D-dimer, ESR
- >3000 WBC or >80% PMNs in synovial fluid
- Elevated synovial alpha-defensin, CRP, or leukocyte esterase
- Intra-operative findings like histopathology, purulence, and a single positive culture
- *Remember that the synovial fluid WBC that defines infection is much lower for PJI vs. native joint septic arthritis*
What is the microbiology of PJI?
- Classic teaching about the micro of PJI defines the groups by time since surgery:
- Both early and delayed infections are from bacteria introduced at surgery
- Early (within 3 months of surgery): tend to be more virulent bacteria like S.aureus and Gram-negative rods
- Delayed (3-12 mo): think more indolent and lower virulence organisms like Cutibacterium and Staph epidermidis
- Late (>1 year out): hematogenous usually, so tend to be from bacteremia organisms like S.aureus, Gram-negatives, and Strep
- Both early and delayed infections are from bacteria introduced at surgery
- *Nico points out that Staph was mentioned in all the categories, so you always have to think about coagulase-negative Staph and S.aureus*
- Nico also emphasized times when you might expect something that isn’t Staph:
- Shoulder PJI is frequently due to Cutibacterium
- Recurrent PJI immediately following a failed course of treatment (think about difficult to treat organisms like VRE or Corynebacterium striatum)
- When the patients has or just had an invasive bacteremic infection with another organism
What are the surgical approaches for PJI?
- Remember that joint prostheses have both fixed metal components (that are hammed/cemented into the patient’s bone) as well as polyethylene lines that attach to the metal components to create the mobile articulating surface at the joint
- Debridement and implant retention (DAIR)
- Also may hear: I&D with poly exchange, I&D with exchange of mobile components, I&D with liner exchange
- Surgeon cuts out infected tissue/bone, removes the polyethylene liner, scrubs/irrigates, and then puts on a new liner and closes
- Pros: Much less invasive than exchange arthroplasty (there is no removal of metal components out of patient’s bone)
- Cons: harder to ensure that all the infected material is out, particularly for infections that have been there for a while or are due to organisms that make a lot of biofilm
- Use for:
- Infections that develop within the first few weeks after surgery (or at least when we’ve caught the infection right after patient started having symptoms)
- When there hasn’t been much time for infection to build up on the metal components
- When no evidence of advanced infection such as hardware loosening on imaging or sinus tract
- When you DON’T have organisms that create biofilm or are hard to treat (aka NOT S.aureus, fungi)
- Often used in patients who might not tolerate an exchange arthroplasty due to comorbidities or overall poor health
- Exchange arthroplasty, which can be single-stage or two-stage procedure
- Entire prosthesis is removed along with all infected tissue
- In single stage: surgeon immediately places a new prosthesis into same site
- In two stage: surgeon first places a cement spacer (often mixed with antibiotics like vancomycin + tobramycin or gentamicin), then comes back a couple months later to remove the spacer and place new prosthesis
- The idea here is that the spacer leeches antibiotics into the joint space and if there is still infection left, we’ll be able to detect and take patient back for another debridement and spacer exchange
- Cons: bigger surgery than DAIR; two-stage approach involves several months where patient has an antibiotic spacer, is non-weight-bearing or partial weightbearing because of space, risk of deconditioning
- As Nico discussed, there is regional variation in how these exchange arthroplasties are used
- In Europe, main approaches are DAIR and single-stage exchange. Two stage less common and used predominantly in high risk or difficult cases
- In the US, two-stage exchange is the norm.
- Entire prosthesis is removed along with all infected tissue
So what’s the deal with these spacers?
- Nico delved into the history behind antibiotic spacers:
- Materials scientists back in the 1980s showed that you could mix antibiotics into acrylic cements, put that into a person or animal, and then have it leach out into tissues in meaningful levels.
- Seems that orthopedic surgeons started adding antibiotics into bone cement and spacers in the 1990s, and then published how that went for their patients. Most did well and major side effects were rare
- So this practice become common place and “standard of care”
- It’s hard to find any comparative studies of spacers with vs without antibiotics. Here’s one meta-analysis that pulled data on antibiotic bone cement (not spacers!):
- Parvizi J, Saleh KJ, Ragland PS, Pour AE, Mont MA. Efficacy of antibiotic-impregnated cement in total hip replacement. Acta Orthop. 2008;79(3):335-341. doi:10.1080/17453670710015229
- One study showed reduction in infection with antibiotic cement, and six other studies were negative >> which when lumped into forest plot came out as positive evidence
- Important to note that you can get detectable serum levels of vancomycin and aminoglycosides from antibiotics spacers! So patients can get AKI and allergic reactions up to and including anaphylaxis from antibiotics in spacers. These are rare, but a valuable reminder that antibiotics in spacers are not totally benign.
Antibiotic selection
- Oral or IV antibiotics?
- Nico discussed the 2019 landmark ID trial called OVIVA: Li HK, Rombach I, Zambellas R, et al. Oral versus Intravenous Antibiotics for Bone and Joint Infection. N Engl J Med. 2019;380(5):425-436. doi:10.1056/NEJMoa1710926
- This compared long-term treatment outcomes of oral versus IV antibiotics for bone and joint infection
- Some context: oral antibiotic therapy has been used for ortho infections in Europe and across the world for decades with good results. Previously there had been multiple comparative studies of oral and IV antibiotics for osteomyelitis showing equivalent outcomes
- Nico discussed that OVIVA added: a well-designed multicenter RCT with long-term follow-up and a lot of PJI and other hardware infections (~¼ had infected hardware; ~10% had hardware placed in an infected site) + large sample size to show non-inferiority of oral antibiotics at a clinically meaningful threshold
- All patients received a week of IV therapy, followed by either more IV or oral antibiotics for the remainder of the patients treatment
- Treatment failure rates were the same between the PO and IV groups (13.2% vs 14.6%, respectively)
- No subgroup clearly benefited from IV vs PO
- There were subgroups that trended towards better outcomes with IV: culture-negative infections, infections with oral agent penicillin
- Downsides to OVIVA design: Specific drugs and doses not recorded > and what drugs being used for what bugs
- Nico’s interpretation: He is happy to use high-dose amoxicillin for Streptococcus or Cutibacterium (low PCN MICs), but he favors another agent for organisms with high MICs like Enterococcus or gram negatives
- Nico discussed the 2019 landmark ID trial called OVIVA: Li HK, Rombach I, Zambellas R, et al. Oral versus Intravenous Antibiotics for Bone and Joint Infection. N Engl J Med. 2019;380(5):425-436. doi:10.1056/NEJMoa1710926
- What are oral antibiotic options for S.aureus PJI, like in this episodes case?
- The best studied combination is a fluoroquinolone + rifampin (don’t want to use either as monotherapy due to rapid resistance concerns)
- Nico noted the high incidence of medication interactions, specifically with rifampin and direct-acting anticoagulants.
- Here is a recent paper showing that having to stop your quinolone during treatment of a bone and joint infection isn’t that rare, although most patients did well: Vollmer NJ, Rivera CG, Stevens RW, et al. Safety and Tolerability of Fluoroquinolones in Patients with Staphylococcal Periprosthetic Joint Infections. Clin Infect Dis. 2021;73(5):850-856. doi:10.1093/cid/ciab145
- He mentioned new data coming out on rifabutin for SA infections that might make drug interactions easier to handle
- Albano M, Karau MJ, Greenwood-Quaintance KE, et al. In Vitro Activity of Rifampin, Rifabutin, Rifapentine, and Rifaximin against Planktonic and Biofilm States of Staphylococci Isolated from Periprosthetic Joint Infection. Antimicrob Agents Chemother. 2019;63(11):e00959-19. Published 2019 Oct 22. doi:10.1128/AAC.00959-19
- Doub JB, Heil EL, Ntem-Mensah A, Neeley R, Ching PR. Rifabutin Use in Staphylococcus Biofilm Infections: A Case Series. Antibiotics (Basel). 2020;9(6):326. Published 2020 Jun 13. doi:10.3390/antibiotics9060326
- Nico noted the high incidence of medication interactions, specifically with rifampin and direct-acting anticoagulants.
- The best studied combination is a fluoroquinolone + rifampin (don’t want to use either as monotherapy due to rapid resistance concerns)
- Another option is trimethoprim-sulfa
- Most experts recommend targeting 10 mg/kg/d of trimethoprim, which can often be 2 DS tabs twice a day or more
- These high doses don’t have comparative data vs the standard dose for osteo
- Nico has anecdotally used 1 DS tab twice a day with good results, but overall doesn’t use TMP-SMX that much given difficulty of lab monitoring, risk of acute kidney injury or hyperkalemia (especially with concurrent ACEi, ARB, or spironolactone use)
- Most experts recommend targeting 10 mg/kg/d of trimethoprim, which can often be 2 DS tabs twice a day or more
- Doxycycline or minocycline is a possibility
- Doxy is relatively poorly studied in ortho infections, though there are patients treated with doxy in OVIVA and did ok in subgroup analysis
- Doxy levels can be decreased with rifampin use
- Other options:
- Clindamycin, often used by pediatric ID physicians with success
- Linezolid, but perhaps more for patients who have gotten through most of their therapy given prolonged courses risk neuropathy, bone marrow suppression
- Cefadroxil in setting of MSSA: first-gen cephalosporin like cephalexin, fairly bioavailable, slightly longer half life that allows BID dosing instead of TID or QID
Antibiotic duration with a 2 stage procedure?
- Many centers typically give an initial 6-week course of antibiotic therapy, followed by a time off antibiotics (“antibiotic holiday”, anywhere from 2-6 wks)
- Many places will trend CRP and/or ESR expecting to see inflammatory markers normalize and then not go up when off antibiotics → Nico points out that this widespread practice isn’t really based on good comparative data.
- The 2011 study mentioned that found CRP trend doesn’t predict treatment outcome: Bejon P, Byren I, Atkins BL, et al. Serial measurement of the C-reactive protein is a poor predictor of treatment outcome in prosthetic joint infection. J Antimicrob Chemother. 2011;66(7):1590-1593. doi:10.1093/jac/dkr182
- There is variation in what docs do after antibiotic holiday:
- Some will do diagnostic arthrocentesis only if CRP is high or rising
- Other groups might just take patient immediately for antibiotic spacer exchange
- Some groups will routinely do arthrocentesis to ensure synovial fluid studies are normal before putting in new prosthesis, even when patients and CRP values are reassuring
- At the time of second stage procedure, surgeons will send new tissue cultures to confirm the infection has been eradicated
- Some centers may also give period of secondary antibiotic prophylaxis to prevent re-infections
What is the role of secondary prophylaxis after 2-stage exchange?
- The prior IDSA PJI guidelines from 2012 suggest there is no role, but the data support this practice are more recent
- Many experts and centers give secondary antibiotic prophylaxis after second stage of exchange arthroplasty based on this RCT by Yang and colleagues from 2020: Yang J, Parvizi J, Hansen EN, et al. 2020 Mark Coventry Award: Microorganism-directed oral antibiotics reduce the rate of failure due to further infection after two-stage revision hip or knee arthroplasty for chronic infection: a multicentre randomized controlled trial at a minimum of two years. Bone Joint J. 2020;102-B(6_Supple_A):3-9. doi:10.1302/0301-620X.102B6.BJJ-2019-1596.R1
- Patients who just completed a 2-stage exchange were randomized to receive either 3 months of oral antibiotics based on prior cultures or no antibiotic prophylaxis.
- Primary outcome was reinfection
- Antibiotic prophylaxis group had less than half the rate of reinfection of the no-antibiotics group (12.5% vs 28.6%), which translates to a number needed to treat of about 6
- Most of the reinfections were with new organisms rather than recurrence of prior infection
- There are some design flaws (such as large proportion of patients excluded from primary analysis), so there hasn’t been widespread consensus on these data changing practice
- One paper mentioned: Kelly MP, Gililland JM, Blackburn BE, Anderson LA, Pelt CE, Certain LK. Extended Oral Antibiotics Increase Bacterial Resistance in Patients Who Fail 2-Stage Exchange for Periprosthetic Joint Infection [published online ahead of print, 2022 Jan 22]. J Arthroplasty. 2022;S0883-5403(22)00044-4. doi:10.1016/j.arth.2022.01.027
- Their early experience with extended antibiotic prophylaxis
- While patients who received prophylaxis had 6% lower rate of treatment failure ( not statistically significant ), two thirds of patients who developed recurrent infection in that group had reinfection with an antibiotic-resistance organisms (vs none of the patients who didn’t get extended prophylaxis)
- Nico explained his approach is to use doxycycline, which is highly active against MSSA, MRSA, and coagulase-negative Staph in his area + well tolerated. They do 2 weeks or until short term follow-up in ID clinic. There is a lot of variability in practice though!!
In the second portion of the episode, the patient received DAIR. In patients who receive DAIR, we give prolonged antibiotic therapy: Typically at least 3 months and 6 months for Staph in an infected knee arthroplasty. In non-Staph infections, some may do as little as 6 weeks after DAIR, but last year there was a large RCT called DATIPO!
- Compared 6 and 12 weeks of therapy in PJI
- Found a large benefit in long-term cure with 12 weeks in the patients who underwent DAIR: 16% absolute risk reduction in DAIR group, which comes out to a number needed to treat of about 6
- So prior to DATIPO, consensus and guidelines-based answer to how long to treat was at least 3 months for Staph…but now we have data to suggest most folks with PJI managed with DAIR should be treated for at least 3 months, even if they have a gram-negative or Strep or other PJI
What about rifampin?
- Patients with retained orthopedic hardware infections with Staph are also recommended to receive a regimen containing rifampin for biofilm eradication if the organism is susceptible
- Most antibiotics target actively dividing cells, which means bacteria just hanging out in biofilm become intrinsically more resistant to most antibiotics vs when they’re not actively multiplying
- Rifampin is unique and goes after RNA polymerase → the idea is that rifampin can eradicate those metabolically quiescent bacteria in biofilm on the hardware and prevent relapse after
- The clinical data that drove adoption of rifampin practice was this RCT: Zimmerli W, Widmer AF, Blatter M, Frei R, Ochsner PE. Role of rifampin for treatment of orthopedic implant-related staphylococcal infections: a randomized controlled trial. Foreign-Body Infection (FBI) Study Group. JAMA. 1998;279(19):1537-1541. doi:10.1001/jama.279.19.1537
- Trial enrolled 33 patients with retained Staph orthopedic hardware infections, including just 15 patients with PJI
- Comparison groups: ciprofloxacin + rifampin vs ciprofloxacin monotherapy (which most docs in 2022 would agree is not appropriate for invasive S.aureus infection)
- A third of the patients in the rifampin arm (which only had 18 patients to begin with) dropped out of the study and weren’t included in the primary analysis, which reported 100$ cure in 12 quinolone-rifampin patients who completed the study protocol vs just 58% of the 12 patients in the quinolone monotherapy arm
- There have been multiple retrospective studies since 1998 which suggest benefit of rifampin based therapy for PJI, but these all suffer from likely selection bias, residual confounding, and other problems that plague retrospective data. Many also don’t stratify outcomes based on antibiotic regimen or include other regimens.
- This 2020 RCT failed to show benefit of rifampin with vancomycin or cloxacillin for Staph PJI: Karlsen ØE, Borgen P, Bragnes B, et al. Rifampin combination therapy in staphylococcal prosthetic joint infections: a randomized controlled trial. J Orthop Surg Res. 2020;15(1):365. Published 2020 Aug 28. doi:10.1186/s13018-020-01877-2
- This 2021 meta-analysis found the sum of evidence did not support benefit of rifampin based regimens: Aydın O, Ergen P, Ozturan B, Ozkan K, Arslan F, Vahaboglu H. Rifampin-accompanied antibiotic regimens in the treatment of prosthetic joint infections: a frequentist and Bayesian meta-analysis of current evidence. Eur J Clin Microbiol Infect Dis. 2021;40(4):665-671. doi:10.1007/s10096-020-04083-4
- Another reminder is that rifampin can have serious drug-drug interactions – so Nico mentioned all of this to say that the literature supporting the absolute recommendation for combination rifampin therapy in Staph PJI is limited, and you could consider avoiding it if there are serious interactions or adverse effects
What about chronic antibiotic suppression after DAIR? Defined as long-term antibiotics after the initial 3-6 mo of definitive treatment.
- Data is all retrospective. There are 3-4 comparative studies that suggest suppressive antibiotics after DAIR for PJI and other ortho hardware infections may reduce long term reinfection risk
- Downsides: pill burden and cost, long-term risk of colonization with antibiotic-resistant bacteria, adverse events of antibiotic themselves
- Nico points out that DATIPO trial patients did not get suppressive antibiotic therapy, and the success rate among those who had DAIR and 12 weeks of antibiotics was >85% (which is not that much worse than the 95% success rate among patients who underwent 2-stage exchange) – so likely most patients who receive DAIR wouldn’t benefit from antibiotic suppression because they’re already going to do well
- Nico approaches suppression after DAIR with shared decision making
- A perspective: Cobo J, Escudero-Sanchez R. Suppressive Antibiotic Treatment in Prosthetic Joint Infections: A Perspective. Antibiotics (Basel). 2021;10(6):743. Published 2021 Jun 19. doi:10.3390/antibiotics10060743
Episode Art & Infographics
Goal
Listeners will be able to describe an approach to the diagnosis and management of prosthetic joint infection
Learning Objectives
After listening to this episode, listeners will be able to:
- Define the common risk factors for prosthetic joint infection (PJI)
- Identify the typical symptoms of PJI and available diagnostic criteria
- Compare and contrast the surgical approaches for PJI
- Recognize and briefly summarize the OVIVA and DATIPO trials
Disclosures
Our guest (Nico Cortes-Penfield) as well as Febrile podcast and hosts report no relevant financial disclosures
Citations
Cortes-Penfield, N., Ryder, J., Dong, S. “#31: Truth or DAIR”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/ff70b6f9-8443-4683-8cce-f3acc40cf2e2