Credits
Host: Sara Dong
Guest: Jill Weatherhead
Writing/Producing/Editing/Cover Art: Sara Dong
Infographics: Hawra Al Lawati, Marcela Santana, Sara Dong
Our Guests
Jill Weatherhead, MD, PhD, cTropMed, FAAP

Dr. Jill Weatherhead is an Assistant Professor of Pediatrics and Medicine in the Sections of Pediatric Tropical Medicine, Pediatric Infectious Diseases and Adult Infectious Diseases at Baylor College of Medicine and Texas Children’s Hospital. She is board certified in internal medicine, pediatrics, pediatric infectious diseases, and adult infectious disease with a sub-specialty certificate in tropical medicine and travelers health. Dr. Weatherhead did her medical training at Michigan State University and her residency and fellowship training at Baylor College of Medicine. She is a physician-scientist and her lab investigates the underlying pathways that cause parasite-induced morbidity and aims to discover interventions that will prevent the development of devastating, life-long disease as a result of parasite infections in children. Dr. Weatherhead is also the Director of Medical Education at the National School of Tropical Medicine (NSTM) at BCM and provides patient care at the Tropical Medicine Clinic as part of the Harris County Health System which services uninsured and underinsured residents in Houston, TX and the Pediatric Tropical Medicine Clinic at Texas Children’s Hospital.
Hawra Al Lawati, MD

Dr. Hawra Al-Lawati was born and raised in Muscat, Oman and went to medical school at Weill Cornell in Qatar. She then moved to Boston for my Internal Medicine residency at Massachusetts General Hospital. She is now an infectious diseases fellow at Beth Israel Deaconess Medical Center (BIDMC) who loves everything ID & MedEd
Marcela Araújo de Oliveira Santana

I am a medical student at Federal University of Uberlândia, completing my final year (6th year). I was born and raised in a small village in Minas Gerais, Brazil. I am hoping to be an internal medicine resident soon with the intent of specializing in infectious diseases! My interests are medical education, infectious diseases (especially tropical diseases), and rural health! I love reading (I am a big fan of dystopias), cooking, and playing board games with my friends.
Culture
Jill loves to be an adventurer! She has been exploring Texas outdoors with her family
Consult Notes
Consult Q
3 yo boy with one month of persistent fevers
One-liner
3 yo previously healthy boy with visceral larva migrans
Key Points
Jump to:
Defining fever of unknown origin (FUO)
- The classic definition of FUO comes from the 1961 study by Petersdorf and Beeson, which included adults with:
- Fever >=38.3C on several occasion
- Duration of fever at least 3 weeks
- Uncertain diagnosis after 1 week in hospital
- This has been refined over time, particularly eliminating the in-hospital evaluation as much of the FUO evaluation can often be done largely in the outpatient setting. The definition has also been adjusted with suggestions to classify based on nosocomial, neutropenic, or HIV and immunocompromised host-associated categories
- In pediatrics, studies of FUO have used various definitions as well. In general though, FUO in children should be considered after minimum of 14 days of daily documented temperatures >38.3C without apparent cause (after repeated physical exams and screening labs)
What information do we need to begin the FUO evaluation? A comprehensive history and physical exam is the first and most crucial step!! Here are some key topics and questions to ask:
- How is the temperature assessed?
- By touch? Thermometer? If thermometer, which type and where?
- Fever noted by both caregiver and others?
- Frequency and timing of fever
- How long, how high, when in the day? Fever diaries are a useful tool to have patients or patient families complete. These should include: date and time of fever, height/duration of fever, method of assessing fever, associated symptoms, response to antipyretics
- When the child is febrile, do they appear ill or have symptoms?
- Does the fever respond to ibuprofen or acetaminophen?
- Do their symptoms persist despite fever resolution?
- Do they sweat with fever?
- Symptoms?
- Red eyes?
- Pharyngitis/sore throat? Mouth ulcers?
- Gastrointestinal complaints?
- Limb or bone pain?
- Medication list! Everything including over the counter supplements
- Sick contacts
- Travel history (back to birth)
- Tick/insect exposures
- Animal contacts
- Diet: any raw meat or seafood? Pica?
Here is a summary of the general initial steps in FUO evaluation.
- Stop all nonessential medications
- CBC, differential, smear
- ESR and CRP
- Aerobic and anaerobic blood cultures
- UA and urine culture
- Chest X-ray
- Serum electrolytes, BUN/Cr
- LFTs
- TB screening
- HIV testing
- After this, can use targeted evaluation based on history, physical exam, results of basic screening tests
- Examples to investigate from ID perspective might include: Brucella, Bartonella, Leptospirosis, Malaria, TB, Salmonella, Toxoplasma, Tularemia, Typhoid fever
- If no cause is identified, you would likely need to consider imaging as well. We won’t dive too far into this here
So what do children with FUO end up being diagnosed with?
FUO is usually caused by common disorders, often with an unusual presentation, and infections have been the most commonly identified causes of FUO in children. This systematic review from 2011 looked at 18 pediatric studies (1638 children) and found an infectious cause for FUO in 51% of children. The infectious causes are outlined in Table 3 of the paper below. Younger children (under 6 yo) were also more likely to have infectious cause of FUO compared to older children.
Thinking about eosinophilia
- As Jill mentioned in the episode, don’t forget to calculate your absolute eosinophil count!! Don’t use just the percentage
- You can grade the severity of eosinophilia based on AEC:
- Mild 500-1500
- Moderate 1500-5000
- Severe >5000
- Important to remember that AEC alone does not predict organ damage or identify the cause!
The differential diagnosis for eosinophilia is very very broad! It can help to think of different buckets of causes:
- Allergic/Atopy
- Asthma, allergic rhinitis, atopic dermatitis
- **Drug hypersensitivity! (such as DRESS, interstitial nephritis)
- ID — more on this next!
- Neoplastic/Malignancy
- Rheumatologic/Autoimmune
- Eosinophilic disorders
The ID differential diagnosis for eosinophilia remains broad as well.
- As Jill noted in the episode, eosinophilia is a reaction to a tissue-invasive helminth → with intensity proportional to degree to tissue invasion. Eosinophils are largely found in tissues, so parasites need to be in contact with host tissue to cause eosinophilia. Depending on the worm lifecycle, it might cause no eosinophilia, acute eosinophilia, or acute and chronic eosinophilia. For example: during the initial larval migration stage after a new infection, there may be intense eosinophilia but this may be mild or absent late in disease.
- Schistosomiasis and Strongyloidiasis are the most common parasitic causes of eosinophilia in a returning traveler.
- If a patient has not traveled out of North America or the US, the list is likely a bit more limited: Strongyloides, Toxocara, ABPA, Coccidioides, scabies, Bartonella, Paragonimiasis (P.kellicotti), dirofilariasis (dog heartworm), resolving scarlet fever. Check out Table 1 here for a nice breakdown based on geographic location, duration of eosinophilia, and main anatomic site of infection!
- Here is a longer list of possible infections grouped by category:
- Helminths/worms
- Flukes (trematodes): Schistosomiasis, Fascioliasis, Opisthorchiasis, Clonorchiasis, Paragonimiasis
- Tapeworms (cestodes): Echinococcosis, Sparganosis
- Roundworms (nematodes): Strongyloides, Trichinella, Filariasis, Toxocariasis, hookworm (e.g. Ancylostoma), Gnathostomiasis, Capillariasis, Anisakiasis, Ascariasis, Onchocerciasis, Loiasis, Trichuriasis
- Ectoparasites
- Scabies
- Myiasis
- Protozoans
- Isospora
- Sarcocystis
- Cystoisosporiasis
- D.fragilis
- Fungi
- Coccidiomycosis
- ABPA
- Histoplasmosis
- Paracoccidioidomycosis
- Cryptococcosis
- Basidiobolomycosis
- Viral
- HIV
- HTLV-1
- Bacterial/Mycobacterial:
- Bartonella
- Syphilis
- TB
- M.leprae
- Helminths/worms
- There is a nice list on the UpToDate article as well that walks through possible findings that may clue you in to particular diagnoses
A few good reads about eosinophilia:
- Highly recommend! → Roufosse F, Weller PF. Practical approach to the patient with hypereosinophilia. J Allergy Clin Immunol. 2010;126(1):39-44. doi:10.1016/j.jaci.2010.04.011
- O’Connell EM, Nutman TB. Eosinophilia in Infectious Diseases. Immunol Allergy Clin North Am. 2015;35(3):493-522. doi:10.1016/j.iac.2015.05.003
- Mejia R, Nutman TB. Evaluation and differential diagnosis of marked, persistent eosinophilia. Semin Hematol. 2012;49(2):149-159. doi:10.1053/j.seminhematol.2012.01.006
- Williams KW, Ware J, Abiodun A, Holland-Thomas NC, Khoury P, Klion AD. Hypereosinophilia in Children and Adults: A Retrospective Comparison. J Allergy Clin Immunol Pract. 2016;4(5):941-947.e1. doi:10.1016/j.jaip.2016.03.020
The featured infection this episode was due to Toxocara! Let’s dive in!
The basics: Life Cycle & Transmission
- Also known as dog roundworm
- Adult roundworms of Toxocara spp live in small intestines of various wild or domestic definitive hosts
- T.canis = dogs! Also coyotes, foxes, wolves
- T.cati, T.malaysiensis = cats!
- Infected definitive hosts (dogs, cats) → excrete eggs in feces into environment
- Under suitable conditions and after ~2-4 wks, embryonation occurs –> these hardy eggs can then remain infective for many months or years
- Eggs are accidentally ingested by humans thru contact with contaminated hands, food, water, or soil
- Later, in the small intestine: larvae released from eggs, penetrate intestinal wall, travel via circulatory system to various organs (lungs, liver, skeletal muscle, heart, brain/eyes/CNS)
- Tissue infection leads to inflammatory immune response, which contributes to local inflammation (increased production of cytokines, eosinophilia/eosinophilic granulomas in host tissues)
- **Larvae can penetrate and hatch in humans, but they are unable to complete their life cycle (like they would in dogs/cats) → so infected humans cannot transmit to others (humans are not excreting eggs!)**
- A less common route of transmission but humans can also be infected by eating undercooked meat with animal infected
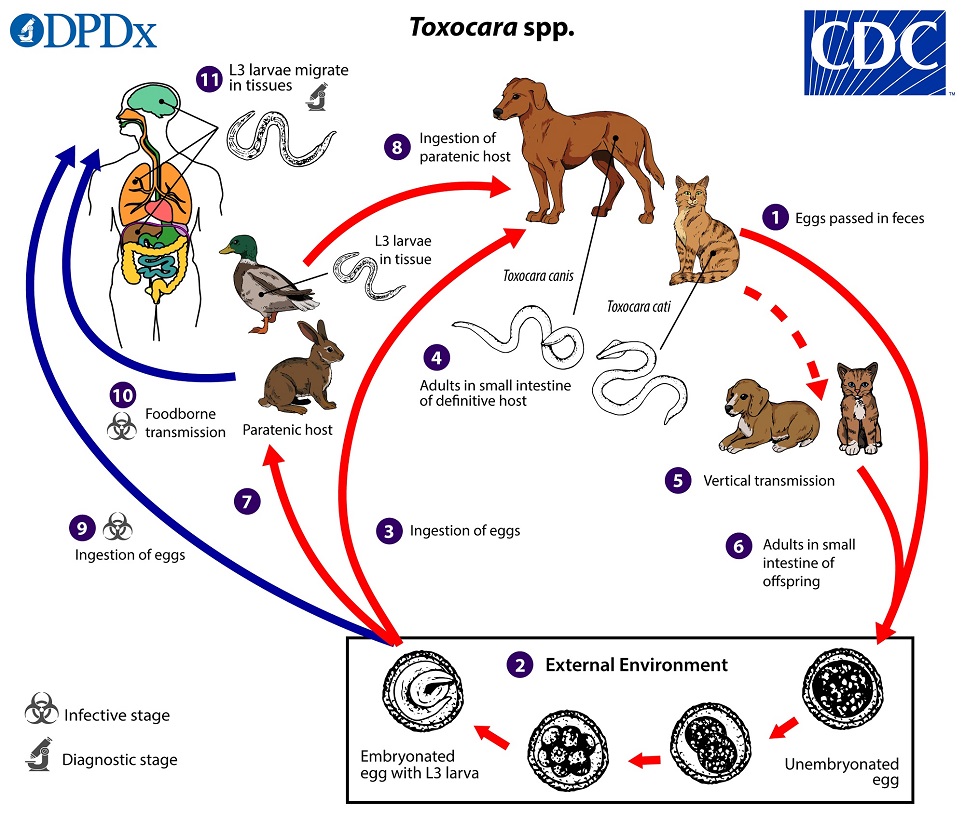
Source: CDC, Parasites-Toxocariasis
Epidemiology
- T.canis and T.cati have worldwide distribution, but despite the large burden, there are still many gaps in our understanding of disease
- Epidemiological information for most countries is still limited. In addition, use of serology in several of the studies is challenging to distinguish exposure vs infection. In the US, Toxocara is not a reportable disease and there are no specific surveillance systems in place to track cases.
- There has been a range of studies looking at seroprevalence with widely variable rates. The overall prevalence estimate for the US in this study was 13.9% for all adults and children over the age of 6: Won KY, Kruszon-Moran D, Schantz PM, Jones JL. National seroprevalence and risk factors for Zoonotic Toxocara spp. infection. Am J Trop Med Hyg. 2008;79(4):552-557
- Risk factors for infection:
- Association with puppies under 3 month
- Tropical or subtropical climates. In the US, southern/southeastern US
- Pica or geophagia (eating soil)
- Male sex
- Low socioeconomic status
- This is both an urban and rural parasite!
- Children are at high risk when they ingest contaminated soil while playing. Common areas include playgrounds, sandboxes, backyards.
- Eggs can also end up in some municipal drinking water supplies and recreational waters
Clinical manifestations
- Asymptomatic or subclinical infection can occur. Severity and presentation of disease depends on the inoculum (how much of the eggs at one time) and where the worms go. The three most common forms of toxocariasis include visceral larva migrans, ocular larva migrans, and neurotoxocariasis.
- Visceral larva migrans
- The most common syndrome in infected people, especially in children under 7 yo
- A febrile illness characterized by eosinophilia and organ involvement
- Most commonly affected organs: lungs and liver
- Pulmonary symptoms can be confused with asthma or viral illness due to cough and wheezing in presentation. May be accompanied by infiltrates on chest imaging
- Liver: abdominal pain, hepatomegaly, lesions on CT
- Other observed locations include myocarditis and nephritis
- See more below on the possible long-term consequences of VLM
- Ocular larva migrans
- Ocular disease is commonly seen in children/teenagers in 8-16yo range, and is due to larval localization in eye with resultant granulomatous inflammation.
- The level of impairment is related to the degree of immune response in the eye. Unilateral visual impairment or strabismus can occur as well as chronic endophthalmitis, retinitis. Blindness can result from severe vitritis, cystoid macular edema, retinal detachment.
- Lesions may closely resemble retinoblastoma
- May or may not have systemic symptoms or eosinophilia that is seen in visceral disease
- Neurotoxocariasis
- Migration of Toxocara larvae into the central nervous system which leads to meningitis, encephalitis, cerebral vasculitis, or myelitis.
- Often associated with nonspecific clinical symptoms.
- This is rare, often affecting middle-aged adults.
- CSF examination would demonstrate eosinophilic pleocytosis
How do patients do?
Infection is usually self-limiting and mild. Death is rare in humans (can be fatal in puppies). When there has been death in humans, attributed to myocardial or CNS involvement with exuberant immune response
Toxocara is increasingly implicated as a risk factor for some long term consequences and morbidity.
- Permanent vision loss and blindness
- There could be a connection between asthma, allergic symptoms, and infection with Toxocara, although still being investigated currently. It’s postulated that larvae in lung may be underlying factor in allergic pulmonary disease and pulmonary fibrosis
- Decreased FEV1 in patients with previous Toxocara infection in NYC: Walsh MG, Haseeb MA. Toxocariasis and lung function: relevance of a neglected infection in an urban landscape. Acta Parasitol. 2014;59(1):126-131. doi:10.2478/s11686-014-0221-7
- 2018 meta-analysis with increased risk for asthma among children with Toxocara infection seropositivity. OR 1.91, 95% CI 1.47-2.47. Aghaei S, Riahi SM, Rostami A, et al. Toxocara spp. infection and risk of childhood asthma: A systematic review and meta-analysis. Acta Trop. 2018;182:298-304. doi:10.1016/j.actatropica.2018.03.022
- Mendonça LR, Veiga RV, Dattoli VC, et al. Toxocara seropositivity, atopy and wheezing in children living in poor neighbourhoods in urban Latin American. PLoS Negl Trop Dis. 2012;6(11):e1886. doi:10.1371/journal.pntd.0001886
- Li L, Gao W, Yang X, et al. Asthma and toxocariasis. Ann Allergy Asthma Immunol. 2014;113(2):187-192. doi:10.1016/j.anai.2014.05.016
- Children with serologic evidence of infection were noted to have measurable reductions in cognitive test scores compared to those without exposure. Infected children were significantly more likely to be in lower socioeconomic class, and the difference in performance persisted when controlled for socioeconomic class → suggesting that toxocariasis may play a role in perpetuating poverty and health disparities in endemic areas
- Implicated in neurodegenerative disorders
- Prior disease has been implicated as a risk factor for epilepsy
- Luna J, Cicero CE, Rateau G, et al. Updated evidence of the association between toxocariasis and epilepsy: Systematic review and meta-analysis. PLoS Negl Trop Dis. 2018;12(7):e0006665. Published 2018 Jul 20. doi:10.1371/journal.pntd.0006665
- Showed significant association:. Arpino C, Gattinara GC, Piergili D, Curatolo P. Toxocara infection and epilepsy in children: a case-control study. Epilepsia. 1990;31(1):33-36. doi:10.1111/j.1528-1157.1990.tb05356.x
- Did not show relationship: Akyol A, Bicerol B, Ertug S, Ertabaklar H, Kiylioglu N. Epilepsy and seropositivity rates of Toxocara canis and Toxoplasma gondii. Seizure. 2007;16(3):233-237. doi:10.1016/j.seizure.2006.12.008
Diagnosis
- Although definitive diagnosis is finding larvae on a pathologic specimen → diagnosis is typically established based on clinical scenario and lab data/serology
- Recommended test for diagnosis (and previous epi studies) is serology: IgG against excretory-secretory Ag, ELISA
- Serologic testing detects immune response to larval form and does not necessarily confirm current active infection!
- Reminder that stool O&P are not useful as larvae do not complete their life cycle in human beings!
Treatment
- Treatment with antihelminthic agent is recommended for acute symptomatic toxocariasis
- Albendazole is preferred, 400mg PO BID x 5d.
- Additionally, ocular disease should be also managed with:
- Ophthalmology referral (select cases may require surgery)
- Treatment with topical and systemic corticosteroids can be beneficial if signs of inflammation
- Other severe infections, such as respiratory, CNS, or cardiac disease, may also require corticosteroids
- We still need large and well defined clinical studies regarding the optimal treatment/dosing/duration for toxocariasis, especially in children
- No recommendations exist for treating asymptomatic patients with positive serology and these patients do not necessarily require treatment.
Prevention & Control
- Enhancing education, increase awareness, educating patients/parents on how to avoid
- Take dogs and cats to vet for routine deworming (especially younger animals)
- Promptly remove dog or cat feces to reduce likelihood of Toxocara egg embryonation
- Keep sandboxes covered as able
- Promote good hand hygiene
- Teach children not to eat soil or sand as much as possible
Check out some references below as well as textbook chapter suggestions in the last section
- A great overview! Ma G, Holland CV, Wang T, et al. Human toxocariasis. Lancet Infect Dis. 2018;18(1):e14-e24. doi:10.1016/S1473-3099(17)30331-6
- Woodhall DM, Fiore AE. Toxocariasis: A Review for Pediatricians. J Pediatric Infect Dis Soc. 2014;3(2):154-159. doi:10.1093/jpids/pit066
- Lee RM, Moore LB, Bottazzi ME, Hotez PJ. Toxocariasis in North America: a systematic review. PLoS Negl Trop Dis. 2014;8(8):e3116. Published 2014 Aug 28. doi:10.1371/journal.pntd.0003116
- Woodhall DM, Eberhard ML, Parise ME. Neglected parasitic infections in the United States: toxocariasis. Am J Trop Med Hyg. 2014;90(5):810-813. doi:10.4269/ajtmh.13-0725
Other miscellaneous mentions and notes:
- Like textbook references?
- Mandell, Principles and Practice of ID, 8th Ed., 9th Ed.:
- Chapter 292: Visceral Larva Migrans and Other Uncommon Helminth Infections
- Long, Principles and Practice of Pediatric ID, 5th Ed.:
- Chapter 277: Tissue Nematodes → Visceral Larva Migrans and Ocular Larva Migrans Caused by T.cani, T.cati, Baylisascaris procyonis
- Chapter 15: Prolonged, Recurrent, and Periodic Fever Syndromes → Fever of Unknown Origin
- Comprehensive Review of Infectious Diseases
- Page 126
- Infections of Leisure. 5th edition. Schlossberg, editor.
- Pages 122-125, 142-143
- Mandell, Principles and Practice of ID, 8th Ed., 9th Ed.:
Episode Art & Infographics
Goal
Listeners will learn the epidemiology, clinical manifestations, diagnosis and management of Toxocara infection.
Learning Objectives
After listening to this episode, listeners will be able to:
- Summarize the critical steps in evaluation of fever of unknown origin and eosinophilia
- Describe the life cycle and transmission of Toxocara spp.
- Identify risk factors for Toxocara infection
- Diagnose and treat visceral larva migrans
Disclosures
Our guest (Jill Weatherhead) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Weatherhead, J., Dong, S. “#6: The Fever and The Worm”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/cdb7af25-5367-4561-bda7-ce5e1d0a36df