Credits
Host: Sara Dong
Guest: Tara Vijayan
Writing/Producing/Editing/Cover Art: Sara Dong
Infographics: Sara Dong
She is an associate professor of medicine in the division of infectious diseases at UCLA. She currently serves as the Medical Director for the Antimicrobial Stewardship Program and also carries several other roles within the School of Medicine including Associate Director of Scientific Foundations of Medicine, Director of the Health Equity Pathway for the Internal Medicine Residency and Director of the Medical Education Pathway for the Multicampus Fellowship in Infectious Diseases. Her passions are health equity, implementation science and combating the global threat of antimicrobial resistance. Outside of UCLA she loves doing puzzles, reading and hiking with her two wildlings, her husband and her 10-year-old hound.
Consult Notes
Consult Q
GPCs in blood cxs
One-liner
50 yo M with history of type A aortic dissection s/p Bentall procedure who was found to have Staph lugdunensis bacteremia and aortic graft infection.
Key Points
Jump to:
- S.lugdunensis introduction and clinical presentations
- S.lugdunensis microbiology notes
- S.lugdunensis antibiotic susceptibilities
- Approach to consideration of possible blood culture contaminants
- Use of nuclear medicine imaging in ID and vascular graft infection
- Other miscellaneous notes and textbook chapters
Staph lugdunensis!
- S.lugdunensis has a special position within the coagulase-negative Staphylococci (CoNS) due to it’s pathogenicity and clinical significance. Unlike other CoNS, S.lugdunensis is known for causing severe and aggressive disease similar to S.aureus.
- First identified in 1980s and is named after Lyon, France where organism first isolated (Lugdunum = Latin name of Lyon)
- Community-acquired and a part of normal skin flora. Often associated with lower body and extremities — particularly in areas like pelvis, perineum, groin, lower extremities, axilla. Can be found in nasal cavity
Clinical Presentations of S.lugdunensis
- Probably most well known for causing destructive infective endocarditis with high mortality rate
- Kyaw H, Raju F, Shaikh AZ, et al. Staphylococcus Lugdunensis Endocarditis and Cerebrovascular Accident: A Systemic Review of Risk Factors and Clinical outcome. Cureus. 2018;10(4):e2469. Published 2018 Apr 12. doi:10.7759/cureus.2469
- Liu PY, Huang YF, Tang CW, et al. Staphylococcus lugdunensis infective endocarditis: a literature review and analysis of risk factors. J Microbiol Immunol Infect. 2010;43(6):478-484. doi:10.1016/S1684-1182(10)60074-6
- Anguera I, Del Río A, Miró JM, et al. Staphylococcus lugdunensis infective endocarditis: description of 10 cases and analysis of native valve, prosthetic valve, and pacemaker lead endocarditis clinical profiles. Heart. 2005;91(2):e10. doi:10.1136/hrt.2004.040659
- Bacteremia, sepsis, and vascular catheter-related infections
- Skin and soft tissue infections: wound infection and abscess, often in perineal and pelvic girdle region
- Bone and joint infections
- PJI
- Fracture fixation devices
- Vertebral osteomyelitis
- Infective arthritis
- Osteomyelitis
- Douiri N, Hansmann Y, Lefebvre N, et al. Staphylococcus lugdunensis: a virulent pathogen causing bone and joint infections. Clin Microbiol Infect. 2016;22(8):747-748. doi:10.1016/j.cmi.2016.05.031
Micro details for S.lugdunensis
- Gram positive, catalase positive, coagulase negative
- May demonstrate hemolysis on BAP
- Colonies: unpigmented, cream-colored, pale yellow to golden
- Pearl: Use of latex agglutination tests for clumping factor to distinguish S.aureus from CoNS → can lead to false ID of S.aureus as it can also agglutinate S.lugdunensis
- Nowadays, MALDI TOF can accurately identify CoNS to spp level
Why is S.lugdunensis so pathogenic / virulent?
- Genomic analysis of S.lugdunensis strains lacked many of virulence factors seen in S.aureus
- We still have a lot to learn about exact mechanisms.
- For a list of virulence-associated factors of S.lugdunensis, check out Table 2 in this Clin Micro Review
- Ability to form biofilm is an important mechanism and a major factor in device-related infection and PJI
Antibiotic susceptibilities in S.lugdunensis
S.lugdunensis isolates are usually known to be susceptible to most antibiotics, unlike many other CoNS (such as S.epidermidis). We discussed this on the show, and here are some notes and references:
Penicillin resistance was reported <4% in 1990s, but appears to be increasing (10-25% range)
Oxacillin/Methacillin
- Resistance to ox/methicillin and most b-lactam antibiotics is conferred by mecA gene, which is acquired by horizontal transfer of mobile genetic elements called staphylococcal cassette chromosome mec elements (SCCmec)
- mecA in S.lugdunensis is uncommon. Ranges from ~3-5% with exception of Taiwan (reported occurrence 21%)
- CoNS isolates that harbor mecA gene can have oxacillin MICs in 0.5-2 range → which is much lower than oxacillin MICs observed in mecA-positive isolates of S.lugdunensis and S.aureus
- The CLSI oxacillin breakpoint for S.lugdunensis was modified in 2005 to more precisely reflect presence of mecA
- CLSI recommends S.lugdunensis MICs be interpreted using S.aureus oxacillin and cefoxitin breakpoints (rather than those used by other CoNS)
- S.lugdunensis isolates with oxacillin MIC <=2 mcg/mL = S; those >=4 mcg/mL = R
- In contrast to other CoNS for which breakpoint for ox S <=0.25 and for oxacillin R >=0.5
- Other resistance mechanisms are also rare, but include a novel mecA homologue, mecC
- MICs for strains with mecC are typically in resistant range for cefoxitin and/or oxacillin
- mecC resistance cannot be detected by tests directed at mecA or PBP2A
Here is a great paper on beta-lactam resistance in S.lugdunensis: McHardy IH, Veltman J, Hindler J, Bruxvoort K, Carvalho MM, Humphries RM. Clinical and Microbiological Aspects of β-Lactam Resistance in Staphylococcus lugdunensis. J Clin Microbiol. 2017;55(2):585-595. doi:10.1128/JCM.02092-16
Other resources and those mentioned above:
- CLSI M100 Performance Standards for Antimicrobial Susceptibility Testing, free online
- Kleiner E, Monk AB, Archer GL, Forbes BA. Clinical significance of Staphylococcus lugdunensis isolated from routine cultures. Clin Infect Dis. 2010;51(7):801-803. doi:10.1086/656280
- Lin JF, Cheng CW, Kuo AJ, et al. Clinical experience and microbiologic characteristics of invasive Staphylococcus lugdunensis infection in a tertiary center in northern Taiwan. J Microbiol Immunol Infect. 2015;48(4):406-412. doi:10.1016/j.jmii.2013.12.010
- Taha L, Stegger M, Söderquist B. Staphylococcus lugdunensis: antimicrobial susceptibility and optimal treatment options. Eur J Clin Microbiol Infect Dis. 2019;38(8):1449-1455. doi:10.1007/s10096-019-03571-6
- Yen TY, Sung YJ, Lin HC, et al. Emergence of oxacillin-resistant Staphylococcus lugdunensis carrying staphylococcal cassette chromosome mec type V in central Taiwan. J Microbiol Immunol Infect. 2016;49(6):885-891. doi:10.1016/j.jmii.2014.11.018
The ASM Editors in Conversation podcast covered susceptibility testing for Staph other than S.aureus not too long ago, check out here
Is this a contaminant?! How to approach possible blood culture contaminants
Ascertain details on the blood cultures
- How many bottles/sets were positive? Site of stick? Aerobic/anaerobic bottle? Can also ask about gram stain shape to get clue of organism
- Often there is focus on the number of positive bottles or the ratio (of positive bottles to total bottles), which may or may not be helpful — our episode emphasized how multiple positive sets is concerning in particular!
- Longer time to positivity is often suggestive of contaminant, although this is tough to utilize unless extreme (such as cultures are positive days later)
How is the patient doing clinically?
- Do they have signs or symptoms that would correlate with infection with the bacteria?
- Do they have risk factors, such as hardware or prosthetic valve/graft/catheter/other material, that may require more consideration of pathogens such as CoNS?
Microbiology!
- See the infographic for a reference of organisms that often come into question regarding contaminant or not.
- Organisms that should always be considered clinically significant in blood culture:
- S.aureus
- S.pneumoniae
- Grp A and B Strep
- H.influenzae
- Gram negatives: Enterobacterales, Pseudomonas, anaerobes
- Fungi, mold
A few references/readings:
- Weinstein MP, Reller LB, Murphy JR, Lichtenstein KA. The clinical significance of positive blood cultures: a comprehensive analysis of 500 episodes of bacteremia and fungemia in adults. I. Laboratory and epidemiologic observations. Rev Infect Dis. 1983;5(1):35-53. doi:10.1093/clinids/5.1.35
- Pien BC, Sundaram P, Raoof N, et al. The clinical and prognostic importance of positive blood cultures in adults. Am J Med. 2010;123(9):819-828. doi:10.1016/j.amjmed.2010.03.021
- Dawson S. Blood culture contaminants. J Hosp Infect. 2014;87(1):1-10. doi:10.1016/j.jhin.2014.02.009
- Pardo J, Klinker KP, Borgert SJ, Trikha G, Rand KH, Ramphal R. Time to positivity of blood cultures supports antibiotic de-escalation at 48 hours. Ann Pharmacother. 2014;48(1):33-40. doi:10.1177/1060028013511229
- Hossain B, Islam MS, Rahman A, et al. Understanding Bacterial Isolates in Blood Culture and Approaches Used to Define Bacteria as Contaminants: A Literature Review. Pediatr Infect Dis J. 2016;35(5 Suppl 1):S45-S51. doi:10.1097/INF.0000000000001106
- Mannino Avila E, Stucky Fisher E, Rhee K. True Versus False Bacteremia in Infants and Children Less Than 3 Years of Age [published online ahead of print, 2018 Aug 13]. Pediatr Emerg Care. 2018;10.1097/PEC.0000000000001585. doi:10.1097/PEC.0000000000001585
- Tweetorial from Varun Phadke on approach to blood cultures: https://twitter.com/VarunPhadke2/status/1186491759230107648
- FOAMid blog on blood culture contaminants: https://foamid.com/2018/02/25/contaminants-vs-true-pathogens-in-blood/
Nuclear medicine imaging can be a resource in diagnosis of complicated infections, such as in our case from this episode.
- A review of the utility for different nuc med images for 5 common ID syndromes (diabetic foot osteomyelitis, vertebral osteomyelitis, prosthetic joint infections, endovascular graft infections, FUO): Censullo A, Vijayan T. Using Nuclear Medicine Imaging Wisely in Diagnosing Infectious Diseases. Open Forum Infect Dis. 2017;4(1):ofx011. Published 2017 Feb 3. doi:10.1093/ofid/ofx011
- Check out Table 1 in particular for an overview of the nuclear medicine studies
Thinking about nuclear medicine imaging for endovascular graft infections in particular:
- CT angiography may be a poor tool, especially if patient recently had surgery
- Tagged WBC scans have been evaluated. As Tara mentioned in the show, the limited resolution may decrease its sensitivity, especially for low-grade infections
- FDG-PET/CT has been used successfully with high sensitivity and specificity
- Talk to your local nuclear medicine imaging team. Choices are often limited by what is available.
Some references:
- Gotthardt M, Bleeker-Rovers CP, Boerman OC, Oyen WJ. Imaging of inflammation by PET, conventional scintigraphy, and other imaging techniques. J Nucl Med. 2010;51(12):1937-1949. doi:10.2967/jnumed.110.076232
- Speziale F, Calisti A, Zaccagnini D, Rizzo L, Fiorani P. The value of technetium-99m HMPAO leukocyte scintigraphy in infectious abdominal aortic aneurysm stent graft complications. J Vasc Surg. 2002;35(6):1306-1307. doi:10.1067/mva.2002.123747
- Fukuchi K, Ishida Y, Higashi M, et al. Detection of aortic graft infection by fluorodeoxyglucose positron emission tomography: comparison with computed tomographic findings. J Vasc Surg. 2005;42(5):919-925. doi:10.1016/j.jvs.2005.07.038
- Machelart I, Greib C, Wirth G, et al. Graft infection after a Bentall procedure: A case series and systematic review of the literature. Diagn Microbiol Infect Dis. 2017;88(2):158-162. doi:10.1016/j.diagmicrobio.2017.03.002
- Zogala D, Rucka D, Ptacnik V, et al. How to recognize stent graft infection after endovascular aortic repair: the utility of 18F-FDG PET/CT in an infrequent but serious clinical setting. Ann Nucl Med. 2019;33(8):594-605. doi:10.1007/s12149-019-01370-9
Other miscellaneous mentions and notes:
- A little reading from a CMR on coagulase-negative Staphylococcus: Becker K, Heilmann C, Peters G. Coagulase-negative staphylococci. Clin Microbiol Rev. 2014;27(4):870-926. doi:10.1128/CMR.00109-13
- The End of Coagulase-Negative Staphylococci? A Micro-Comic Strip
- Like textbook references?
- Mandell, Principles and Practice of ID, 8th Ed., 9th Ed.:
- Chapter 197: Staphylococcus epidermidis and other coagulase-negative Staphylococci
- Long, Principles and Practice of Pediatric ID, 5th Ed.:
- Chapter 116: Staphylococcus epidermidis and other coagulase-negative Staphylococci
- Comprehensive Review of Infectious Diseases
- Mandell, Principles and Practice of ID, 8th Ed., 9th Ed.:
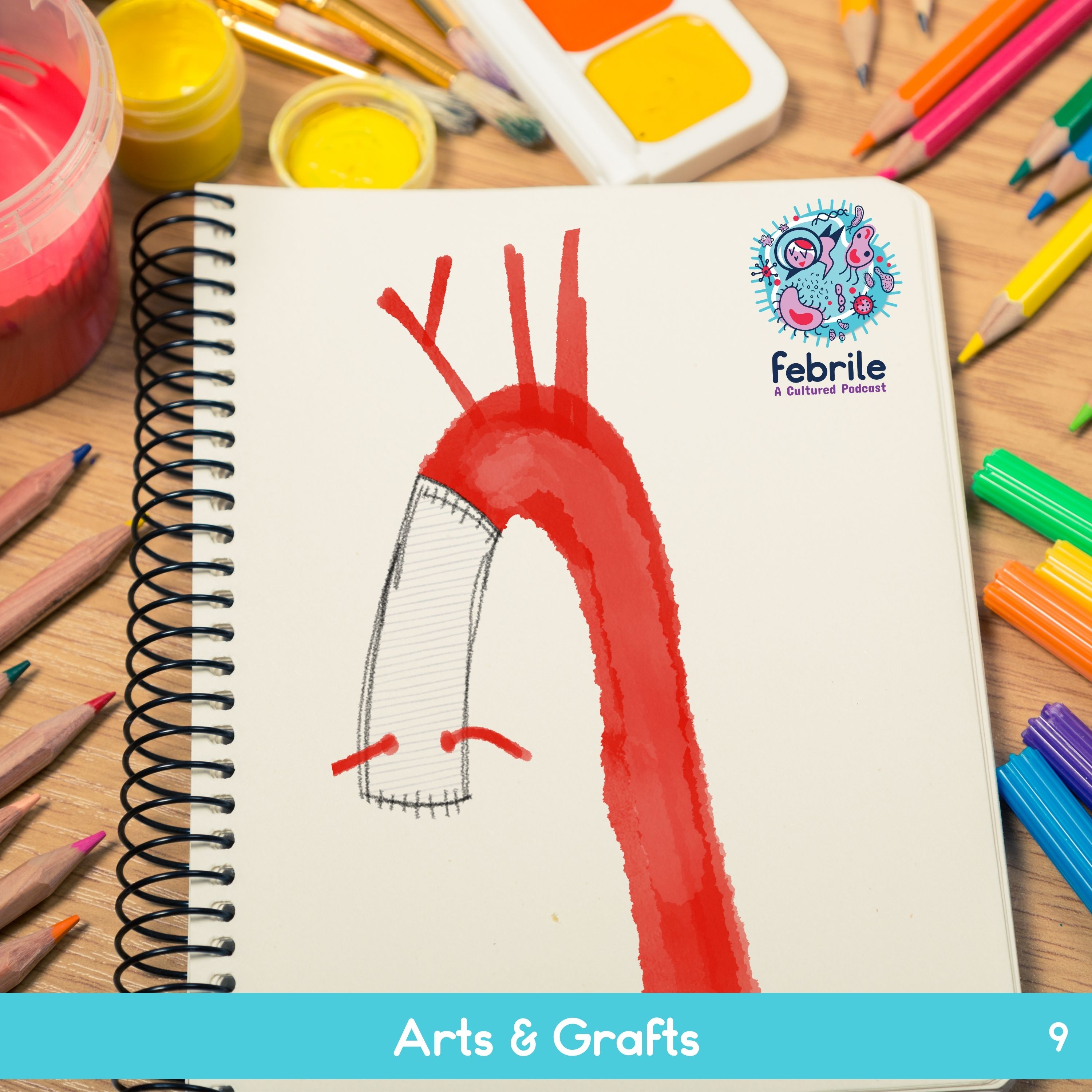
Episode Art & Infographics
Goal
Listeners will be able to identify Staphylococcus lugdunensis as a pathogen with unique characteristics similar to S.aureus
Learning Objectives
After listening to this episode, listeners will be able to:
- Describe common clinical presentations of S.lugdunensis
- Interpret S.lugdunensis antibiotic susceptibilities
- Explain an approach to determining whether a positive blood culture organism is a contaminant
- Discuss the utility of nuclear medicine imaging in the diagnosis of vascular graft infection
Disclosures
Our guest (Tara Vijayan) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Vijayan, T., Dong, S. “#9: Arts & Grafts”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/3c0e8b47-011c-4237-ab6a-5c14c6585134





1 thought on “Episode #9 – Arts & Grafts”
Pingback: Holding True – Research Rendezvous
Comments are closed.