Table of Contents
Credits
Hosts: Nahid Hiermandi, Sara Dong
Guest: Kristen Valencia Deray
Writing: Nahid Hiermandi, Kristen Deray
Producing/Editing/Cover Art/Infographics: Sara Dong
Our Guests
Nahid Hiermandi, DO
Nahid Hiermandi is currently a third year pediatric ID fellow at Baylor College of Medicine/Texas Children’s Hospital in Houston, TX. She did her residency at Phoenix Children’s Hospital. She is currently applying for jobs!
Kristen Valencia Deray, MD

Kristen Valencia Deray is an Assistant Professor in Pediatric Infectious Diseases at Baylor College of Medicine / Texas Children’s Hospital in Houston, TX. She completed her pediatric residency at Nationwide Children’s Hospital followed by her pediatric ID fellowship at Baylor.
Culture
Nahid still loves to stroll through the public library and she shared “The Overstory” by Richard Powers (about trees and environmental activism)
Kristen shared that she is a Swiftie and how fun the Eras tour was!
Consult Notes
Case Summary
Adolescent male with cystic fibrosis s/p bilateral lung transplant who developed fever, cough, and progressive respiratory distress with hypoxia and was found to have disseminated CMV infection (including pneumonitis, retinitis, and cerebritis). Of note, he did have ganciclovir resistance detected with mutation at UL97 site.
Key Points
We have previously covered CMV on the podcast, you can check out prior Febrile episodes on CMV:
- #33 Troll of Transplantation Part 1 on a case of CMV colitis (discusses general overview of CMV in transplant and prevention strategies)
- #35 Troll of Transplantation Part 2 on refractory/resistant CMV
- #37 Curious Congenital Conundrums – Stop, Look, and Listen on congenital CMV
A reminder about some important resources available regarding CMV infection and transplant!
We have previously covered CMV in detail in the Consult Notes above, but just as quick reminders from this episode as well on defining CMV infection vs disease
- While most of these definitions are actually designed for clinical trials (to agree on standardized definitions that would allow studies to be comparable), these definitions are also important for our daily clinical practice, particularly to guide us in our diagnostic approach
- CMV infection is defined as virus isolation or detection of viral proteins or nucleic acid in any body fluid or tissue specimen
- When this specimen is the blood (plasma, serum or whole blood), we talk about viremia (culturing the virus from the blood), antigenemia (pp65 antigen detection) or DNAemia (detection of CMV DNA, the most common technique nowadays)
- CMV disease includes:
- End organ disease caused by CMV, such as pneumonia, GI disease, hepatitis, retinitis, etc
- CMV syndrome, which is an entity only described in SOT (not in HSCT) and includes detection of CMV in the blood with at least two of the following: fever, new/increased malaise/fatigue, leukopenia or neutropenia, atypical lymphocytes, thrombocytopenia, elevated AST or ALT to 2x ULN.
- You can also find these definitions summarized in AST ID COP Guidelines Table 1
A few notes related to pediatric-specific issues in management of CMV
- Most of the basic principles for management and prevention of CMV will be similar to adults, but here are a few important notes.
- Remember that most of the literature on CMV prevention and treatment is in adults and extrapolated to children
- A risk factor for CMV disease is young age, specifically being less than one year old at the time of transplant
- These young children have fewer opportunities for CMV exposure and will likely be recipient negative going into transplant (cohort studies suggest there are more CMV-seronegative pediatric SOT patients than adults → so larger group are at risk for primary and potentially severe CMV disease)
- CMV D+R- children are also at risk for de novo CMV infection acquisition as a result of community exposures such as day care
- All children <1 yo should be considered CMV negative at the time of transplant unless CMV PCR is positive (as any positive immunoglobulin is likely maternal antibody)
- Detection of CMV-specific T-cells is another way to indicate baseline CMV status in children awaiting organ transplant when interpretation of CMV serology is confounded by maternal IgG
- Dosing of valganciclovir in children should be based on body surface area and renal function according to the current AST ID COP guidelines
- Optimal dosing of valganciclovir is controversial, and some centers may use body weight dosing rather than BSA. Here is a recent paper on BW vs BSA dosing in children: Demirhan S, Munoz FM, Valencia Deray KG, Bocchini CE, Danziger-Isakov L, Blum S, Sharma TS, Sherman G, Boguniewicz J, Bacon S, Ardura MI, Maron GM, Ferrolino J, Foca M, Herold BC. Body surface area compared to body weight dosing of valganciclovir is associated with increased toxicity in pediatric solid organ transplantation recipients. Am J Transplant. 2023 Dec;23(12):1961-1971. doi: 10.1016/j.ajt.2023.07.013. Epub 2023 Jul 26. PMID: 37499799.
CMV pneumonitis management in lung transplant recipients
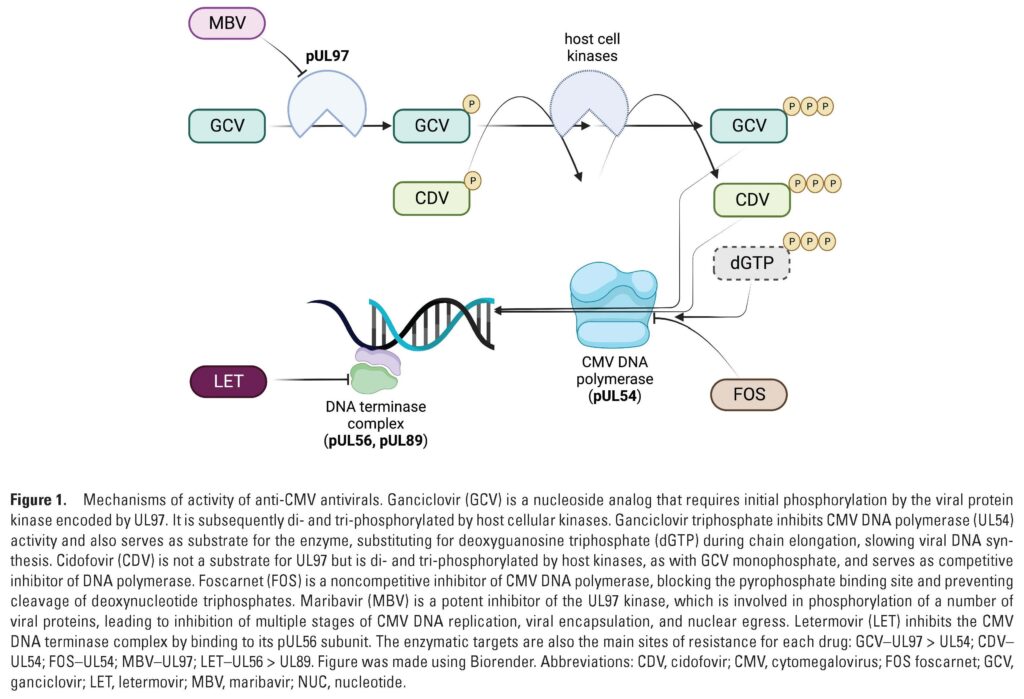
- Available agents for treatment of CMV disease include:
- Ganciclovir or valganciclovir
- For those who cannot tolerate ganciclovir or valganciclovir or those who fail to respond to these agents, second line agents include foscarnet or cidofovir
- Maribavir is a relatively newer agent used for refractory or resistant post-transplant CMV
- See the link below for some further reading
- More information on general treatment is also available in Consult Notes for Episode #33
- We’ll also add a little more information about CMV pneumonitis given the example case in the episode
- Treatment of any symptomatic CMV disease including pneumonitis generally involves both reduction of immunosuppression with antiviral therapy
- Reduction of immunosuppression should be cautiously reduced as able in discussion between the TID and Transplant teams. Ultimately this is done on a case-by-case basis but a few factors that often weigh strongly include:
- Moderate to severe disease
- High viral loads
- Slow clinical or virologic response to antivirals
- Ganciclovir-resistant CMV
- High net state of immunosuppression
- For CMV pneumonitis and tissue-invasive disease, first line treatment is IV ganciclovir (5 mg/kg IV Q12h, adjusted for renal dysfunction)
- GCV can be transitioned to oral valganciclovir once patient has clear clinical improvement, downtrending viral loads, and if able to tolerate oral medications
- Treatment of pneumonitis is similar to other end-organ disease and based on clinical and virologic response to therapy
- The use of adjunctive CMV immune globulin (CytoGam) to antiviral therapy might theoretically improve treatment response, but data supporting use are limited. As Kristen noted, this is not routinely used for treatment
- Reduction of immunosuppression should be cautiously reduced as able in discussion between the TID and Transplant teams. Ultimately this is done on a case-by-case basis but a few factors that often weigh strongly include:
- As Kristen mentioned, the data on therapy for CMV retinitis largely comes from the HIV/AIDS literature
- Intravitreal therapy for CMV retinitis is usually used in combination with systemic therapy for patients with sight-threatening disease → so you’ll be speaking with your ophthalmology colleagues about the need for possible intravitreal antivirals
- Secondary prophylaxis was also mentioned – there are no prospective randomized trials of secondary prophylaxis for prevention of recurrent CMV infection in solid organ transplant recipients after resolution of CMV disease
- Different clinicians and transplant centers may have different approaches and usually have defined their own local threshold on when to trigger therapy
- Here is a recent review of antiviral agents for pediatric transplant recipients: Valencia Deray KG, Danziger-Isakov LA, Downes KJ. Current and Emerging Antiviral Agents in the Prevention and Treatment of Cytomegalovirus in Pediatric Transplant Recipients. J Pediatric Infect Dis Soc. 2024 Feb 28;13(Supplement_1):S14-S21. doi: 10.1093/jpids/piad059. PMID: 38417084; PMCID: PMC10901473.
- Below you can see Figure 1 from this article on mechanisms of activity of anti-CMV antivirals
Ganciclovir resistance
- In this case, Kristen and Nahid discuss using foscarnet and the patient ultimately found to have genotypic resistance testing with mutation at UL-97. Also check out Episode #35 for more on resistance/refractory disease
- Resistance to ganciclovir should be considered if transplant recipient:
- Fails to improve clinically and/or virologically after 2 weeks of adequately dosed antiviral therapy
- Has recurrent relapses following treatment
- Important factors that increase risk of GCV resistance include:
- Prolonged antiviral use (previous antiviral exposure >3 months)
- Lack of prior CMV immunity (CMV D+R- serostatus)
- Inadequate antiviral drug selection of dosing
- Resistance testing should be performed with suspected GCV resistance
- In patients who have been treated with GCV, most common mutation = UL97 phosphotransferase
- The degree of resistance conferred will vary among UL97 mutations
- Sometimes this resistance can be overcome with higher dose GCV but in most cases, treatment with a different antiviral is necessary
- UL54 DNA polymerase mutations may also occur, usually as second mutations in patients who already have UL97
- Alone, a UL54 mutation isn’t necessarily associated with clinical antiviral resistance
- The combination of UL97 and UL54 mutations in CMV isolates though often have high level GCV resistance
- Check out Episode #35 Consult Notes for more details
- In patients who have been treated with GCV, most common mutation = UL97 phosphotransferase
- Treatment of GCV resistant CMV
- The approach will vary based on disease severity, gene mutation present, antiviral drugs available, host immune status
- Reduction of immunosuppression is important
- Typically will use foscarnet. Important to monitor closely for nephrotoxicity and electrolyte disturbances
- Cidofovir is another option although there is less clinical experience and most severe nephrotoxicity potential
- Final antiviral will ultimately be adjusted based on results of your genotypic resistance testing
Just a few additional miscellaneous pearls from the episode related to infections
Rhodococcus equi
- A Gram positive bacteria that exists in soil
- Typically a veterinary pathogen but has been increasingly appreciated as a rare cause of infectionand substantial morbditiy in immunocompromised patients
- Pulmonary infections are the most common form of human disease although extrapulmonary disease can occur (particularly CNS-pulmonary syndrome in an immunocompromised host)
- Typically described as subacute pneumonia that results in high fevers, cough, and fatigue. Hemoptysis can occur as well.
- Malakoplakia (rare chronic granulomatous condition) can also occur in setting of R.equi infection → would appear as dense tissue infiltrate with sheets of foamy histiocytes with abundant coccobacilli and calcific inclusions
- Associated commonly with horses, foals have a unique susceptibility
Chlamydia psittaci
- Associated with contact with birds (documented in many different species – but most humans are infected from birds of the order Psittaciformes, such as parakeets, cockatiels, cockatoos, parrots)
- Usually presents as abrupt fever, headache, and dry cough (think atypical pneumonia with a pronounced headache). More severe disease and other organ system complications are possible though
- Incubation period is between 5-14d usually
Bordetella bronchiseptica
- Cause of kennel cough in dogs, snuffles in rabbits, and atrophic rhinitis in piglets
- Human infection has been documented rarely with presentations ranging from mild respiratory illness to pneumonia and sepsis
- Typically described in immunocompromised individuals exposed to farms or pets
- There have also been rare confirmed cases of vaccine-derived B.bronchiseptica infections (ex: immunocompromised pet owner whose dog receives live vaccine)
Infographics
Goal
Listeners will be able to approach a pediatric solid organ transplant recipient with suspected resistant CMV infection
Learning Objectives
After listening to this episode, listeners will be able to:
- List risk factors for CMV disease in pediatric solid organ transplant recipients
- Describe the expected decline in viral load in response to appropriately dosed antiviral therapy
- Discuss genotypic resistance testing for CMV
Disclosures
Our guests (Nahid Hiermandi and Kristen Valencia Deray) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Hiermandi, N., Deray, K., Dong, S. “#91: Troll of Transplantation 3”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/f5a2be84-b0fd-4562-acd2-1a9e9d276d8f