Table of Contents
Credits
Hosts: Michael Moran, Sara Dong
Guest: Swapnil Lanjewar
Writing: Swapnil Lanjewar
Content Editing, Infographics, Cover Art: Sara Dong
Audio Edit/Mixing: Bentley Brown
Produced by Sara Dong with support from the Infectious Diseases Society of America (IDSA)
Our Guests
Michael Moran, DO, MS

Michael Moran is currently a first year infectious disease fellow at the University of Wisconsin in Madison interested in infection control and the immunocompromised host. He completed internal medicine residency at Riverside Methodist Hospital in Columbus, Ohio and received his DO at Ohio University.
Swapnil Lanjewar, MD, FACP

Swapnil Lanjewar is a clinical Assistant Professor in Infectious Disease at the University of Wisconsin, Madison. He completed his medical schooling in India and pursued his IM residency at the Cleveland Clinic in Ohio. He did his fellowship in Infectious Disease at UW Madison and later stayed back there as a faculty there. His professional interests include NTM and transplant infections and he is also interested in medical education.
Culture
Michael shared taking a mind break by watching 90 Day Fiance
Swapnil shared his love of table tennis
Consult Notes
Case Summary
47 year old female hospitalized due to fever of unknown etiology and new rash, ultimately diagnosed with DRESS likely related to sulfasalazine.
Key Points
Swapnil shared his approach to a call for fever with rash
There is a huge differential for these cases, and Swapnil emphasized the importance of using a structured and organized approach. He likes to allow the team to finish telling the story without interruptions. Although fever and rash is often associated with infectious diseases, there are plenty of noninfectious processes that can present with fever and rash.
He described this approach in 3 stages (more on this below), but the most important is to use a systematic approach that works for you!
1) Before seeing the patient
- How sick is the patient? Are they immunocompromised?
- Is this a surgical disease or emergency such as necrotizing fasciitis?
- Is this a hemorrhagic rash from septicemia secondary to:
- Perforated viscus/bad pyomyositis/huge abscess?
- Toxic shock from retained foreign body (such as tampon)?
- Line or device infection with septic shock?
- If the season and location are right, also consider severe tickborne infections such as babesia, Rocky Mountain Spotted fever (RMSF)
- Fungal infections? Particularly in the immunocompromised population
- Do they need prompt isolation?
- Meningococcal disease, viral hemorrhagic fevers (if appropriate epidemiologic risk factors), patient with transmissible TB?
- Is this exotic disease?
- Is this malaria?
- Travel related?
- Technically, a textbook approach is to also think of bioterrorism but hopefully this is unlikely
- Other considerations to remember:
- Age of the patient
- Season of the year
- Immunization history
2) While seeing the patient
- History taking
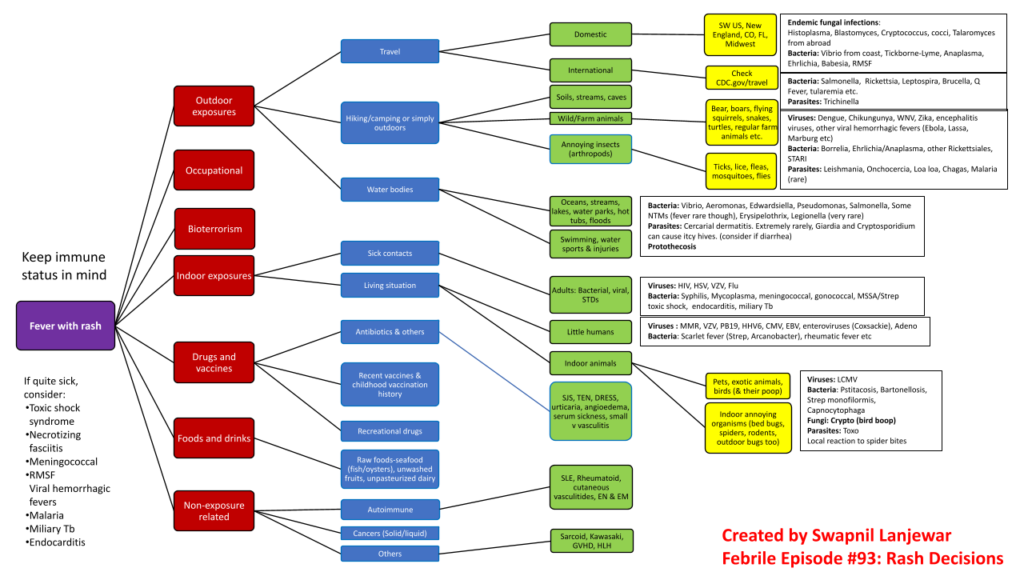
- A careful and thorough history is an extremely important skill in ID. Swapnil likes to follow a personal template with has exposures broken into 5 broad categories:
- Occupational exposures
- Outdoor exposures
- Indoor exposures
- Ingestion/injection exposures
- Non-exposures
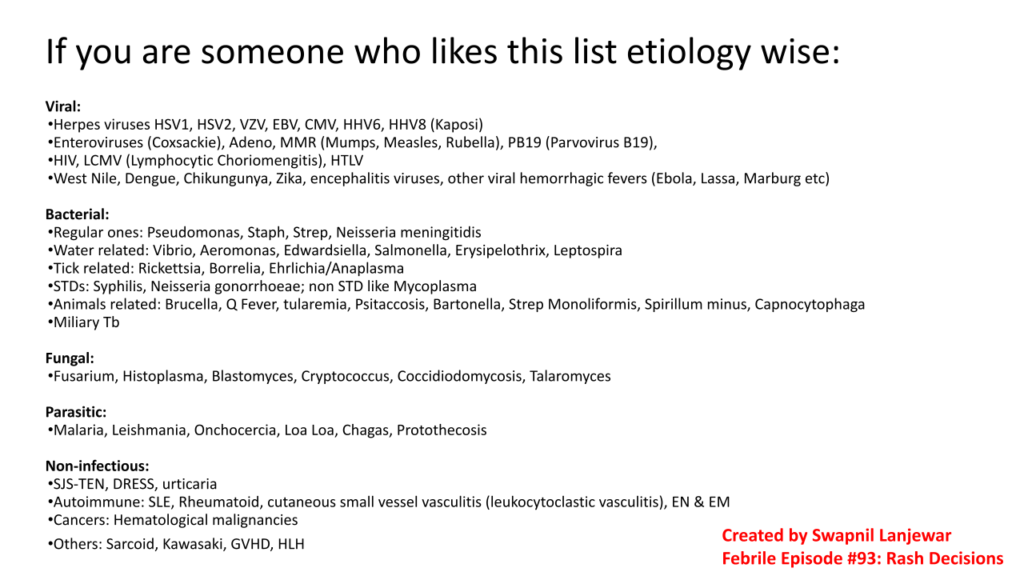
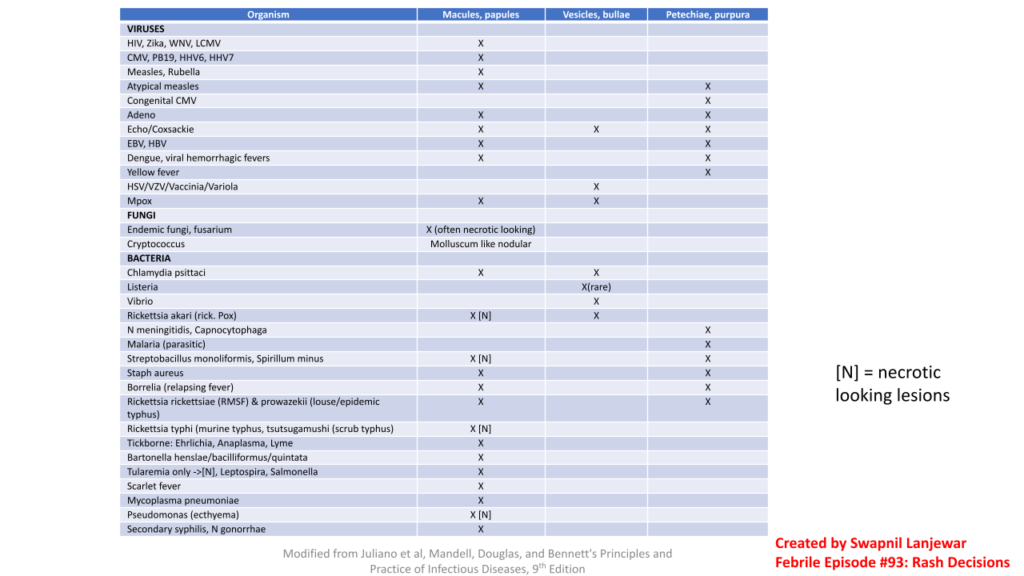
- Here is a chart and list that Swapnil created covering his discussion from the podcast
- A careful and thorough history is an extremely important skill in ID. Swapnil likes to follow a personal template with has exposures broken into 5 broad categories:
- Examination
- The appearance of rash is important to help adjust the infectious differential!! Features of the rash to consider include:
- Characteristics of the lesion(s) – individually and as a group
- Morphology/arrangement such as annular, linear, serpiginous, dermatomal
- Distribution: isolated vs generalized, bilateral vs unilateral, symmetric, occurring on exposed areas
- Distribution and progression of rash
- Evolution such as centrifugal vs centripetal
- Timing of onset in relation to fever
- Secondary features or change in morphology, such as papules to vesicles or petechiae
- Symptoms associated with rash (such as pain, itchiness, numbness)
- Characteristics of the lesion(s) – individually and as a group
- Primary features/definitions:
- Macule – flat, nonpalpable, circumscribed lesion ≤1 cm
- Patch – Flat, nonpalpable, circumscribed lesion >1 cm
- Papule – Elevated, palpable, circumscribed, solid, < 1cm
- Plaque – Elevated, palpable, circumscribed, solid > 1cm, elevation 2/2 ↑ thickness of epidermis
- Papule + fluid → Vesicle
- When vesicle >1cm = Bullae
- Papule + pus = Pustule
- Nodule – Deep-seated (from dermis), roundish, usually >1cm
- Maculopapular – Confluent, erythematous rash made up of both macular and papular lesions
- Purpura – Papular/macular non-blanching lesions secondary to RBC extravasation; petechiae if 1-2mm
- Secondary features (develop as evolution of primary features):
- Crust: dried serum, blood, pus over rash
- Scale: hyperkeratosis
- Excoriation|Fissure|Ulcer|Infarct
- Ulcer – Loss of the epidermis and upper layer of the dermis, resulting in a depressed skin lesion
- Eschar – Hard, black-colored adherent necrotic skin, often overlying an area of ulceration
- Primary/Secondary features above: Modified from textbook of Dermatology, Edited by Jean L. Bolognia , Julie V. Schaffer, Lorenzo Cerroni Fourth edition, China: Elsevier, 2018, ISBN 978–0-7020–6275–9
- Important physical exam features to focus on outside of the skin exam also include:
- Vital signs
- General appearance – ill appearing?
- Lymph nodes, mucous membranes, conjunctivae, genitalia
- Liver/spleen size
- Joint exam
- Meningeal signs / Neurologic exam
- The appearance of rash is important to help adjust the infectious differential!! Features of the rash to consider include:
3) After seeing the patient
- Adjust your differential based on the information you have gathered
- Don’t forget to incorporate lab and imaging results → and consider additional evaluation you may request based on your hypothesis
ID fever and rash emergencies
- There are a few associations of fever, rash, and infection that would be an emergency, so remember these!
- Meningococcemia
- Necrotizing skin and soft tissue infection
- Toxic shock syndrome
- Miliary TB
- Rocky Mountain spotted fever
- Fungal infections in immunocompromised hosts
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome
- Also known as DIHS – drug induced hypersensitivity syndrome
- A rare, severe and potentially life threatening adverse drug reaction characterized by an extensive rash with visceral organ involvement, lymphadenopathy, and usually eosinophilia and atypical lymphocytosis
- DRESS is a T-cell mediated hypersensitivity reaction +/- herpesviridae (HHV-6/CMV/EBV) reactivation with antiviral immune response, although the exact pathogenesis is a bit unclear
- Typically occurs 2-8 weeks after exposure, although latency could be shorter in some cases
- Manifestations:
- Morbilliform rash is typically described but cutaneous and mucosal manifestations can vary. Mucosal involvement in seen in up to half of cases
- Hematologic abnormalities
- Eosinophilia (~80-90% of cases)
- Atypical lymphocytes (35-67% of cases)
- Fever (in most patients)
- Lymphadenopathy
- Facial, hand, foot swelling
- Visceral involvement: can vary in extent and type or organ, but generally patients will have at least one internal organ involvement
- Liver injury is most common, but kidney, pulmonary, cardiac, or other organ involvement is possible
- A clear drug trigger is identified in most cases (~80%), and risk of DRESS varies between drugs. Common culprits / high risk drugs implicated include:
- Aromatic antiepileptic drugs such as phenytoin, carbamazepine, lamotrigine, oxcarbazepine, phenobarbital
- Sulfa drugs/antibiotics (sulfasalazine, dapsone, trimethoprim-sulfamethoxazole, sulfadiazine)
- Allopurinol
- Tetracyclines, especially minocycline
- Vancomycin
- Kardaun SH, Sekula P, Valeyrie-Allanore L, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br J Dermatol. 2013;169(5):1071-1080. doi:10.1111/bjd.12501
- There may be an association between DRESS risk and HLA haplotypes and genetic variants
- Phillips EJ, Chung WH, Mockenhaupt M, Roujeau JC, Mallal SA. Drug hypersensitivity: pharmacogenetics and clinical syndromes. J Allergy Clin Immunol. 2011;127(3 Suppl):S60-S66. doi:10.1016/j.jaci.2010.11.046
- Cho YT, Yang CW, Chu CY. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): An Interplay among Drugs, Viruses, and Immune System. Int J Mol Sci. 2017;18(6):1243. Published 2017 Jun 9. doi:10.3390/ijms18061243
- Konvinse KC, Trubiano JA, Pavlos R, et al. HLA-A*32:01 is strongly associated with vancomycin-induced drug reaction with eosinophilia and systemic symptoms. J Allergy Clin Immunol. 2019;144(1):183-192. doi:10.1016/j.jaci.2019.01.045
- Some commonly used criteria to evaluate diagnosis of DRESS include the Registry of Severe Cutaneous Adverse Reactions (RegiSCAR) scoring system, which includes:
- Fever
- Lymphadenopathy
- Atypical lymphocytes
- Eosinophilia
- Skin involvement (extent, path)
- Internal organs involved
- Resolution timeline > 15 days
- Treatment
- First line:
- STOP the offending drug!!
- Supportive care if mild disease
- If severe, consider glucocorticoids 0.5-1 mg/kg/day, taper over 8-12 weeks
- Remember to give PJP prophylaxis if appropriate with steroid use
- Second line:
- Cyclosporine
- IVIG
- Other immunosuppressive agents such as JAK inhibitors
- First line:
Swapnil also briefly touched on HLH (hemophagocytic lymphohistiocytosis)
- Rare, life-threatening hyperinflammatory syndrome where in there is intense immune activation characterized by fever, cytopenias, hepatosplenomegaly, and highly elevated inflammatory markers
- Can be seen in pediatric or adult patients
- There are genetic and acquired causes. Experts have favored not using terms such as “primary HLH” and “secondary HLH”
- Pathogenesis (oversimplified version!):
- Absence of normal downregulation of activated macrophages and lymphocytes
- Immune dysregulation in cytotoxic pathway of NK and/or cytotoxic T lymphocytes → very high cytokine levels → accumulation of activated lymphocytes and activates macrophages (histiocytes)
- The macrophages can phagocytose host cells including blood components (RBCs, WBCs, platelets), hence the term ‘hemophagocytic’
- Can see in biopsy from bone marrow, spleen, lymph node, liver (immune tissues)
- Diagnostic criteria – need 5 out of 9:
- Fever ≥38.5°C
- Splenomegaly
- Peripheral blood cytopenia, with at least two of the following: hemoglobin <9 g/dL (for infants <4 weeks, hemoglobin <10 g/dL); platelets <100,000/microL; absolute neutrophil count <1000/microL
- Hypertriglyceridemia (fasting triglycerides >265 mg/dL) and/or hypofibrinogenemia (fibrinogen <150 mg/dL)
- Low or absent NK cell activity
- Ferritin >500 ng/mL
- Elevated soluble CD25 (soluble IL-2 receptor alpha [sIL-2R]) two standard deviations above age-adjusted laboratory-specific norms
- Elevated CXCL9
- Hemophagocytosis in bone marrow, spleen, lymph node, or liver
Infographics
Goal
Listeners will be able to discuss infectious and noninfectious etiologies of fever and rash
Learning Objectives
After listening to this episode, listeners will be able to:
- Describe a systematic approach to history and physical exam evaluation for a patient with fever and rash
- List key features of DRESS syndrome, including common antibiotic culprits
Disclosures
Our guests (Michael Moran and Swapnil Lanjewar) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Moran, M., Lanjewar, S., Dong, S. “#93: Rash Decisions”. Febrile: A Cultured Podcast.https://player.captivate.fm/episode/2fe7bc5d-2649-4cc6-894c-46e149f772c2