Table of Contents
Credits
Host(s): Jack Flores, Sara Dong
Guests: Madan Kumar
Writing: Jack Flores
Content Editing, Cover Art: Sara Dong
Audio Editing: Bentley Brown
Produced by Sara Dong with support from the Infectious Diseases Society of America (IDSA)
Our Guests
John “Jack” Flores, MD

Dr. John “Jack” Flores is a third year Med-Peds ID fellow at the University of Chicago who is passionate about all infectious diseases, but sees himself as an academic MedPeds ID provider focusing on adolescent/young adult and maternal-fetal infections along with HIV syndemic care and travel medicine.
Madan Kumar, DO

Dr. Madan Kumar is a pediatric infectious diseases specialist and Assistant Professor in Pediatrics at the University of Chicago’s Comer Children’s Hospital. His various scholarly focuses are with immunocompromised hosts, the intersection of infectious diseases and immune dysregulation, and the study of the microbiome.
Culture
Madan is an amateur woodworker and has recently made some furniture and basic wooden toys
Jack shared his dabbling in riddle-making! Check it out below:
I can be a tree, a bridge, a lily pond, a battle, or a shelf,
Pieces of fruit, a chair, a woman, or even God himself,
These are just a few of the things that often make me sublime,
I’m simply a snapshot of someone’s emotions and perceptions of their world at that time,
Most of the time I’m free, but occasionally I’ll be a pretty price to pay
You can find me almost anywhere, from Dublin to New York, Paris to Mumbai
Solution: A painting!
Consult Notes
Case Summary
2 year old boy who presents with fever and was diagnosed with Kawasaki disease
Key Points
Resources related to KD:
- AAP Red Book: 2021-2024 Report, 32nd edition: Kawasaki Disease chapter
- 2017 American Heart Association Guidance: McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association [published correction appears in Circulation. 2019 Jul 30;140(5):e181-e184]. Circulation. 2017;135(17):e927-e999. doi:10.1161/CIR.0000000000000484
- 2021 American College of Rheumatology Guideline: Gorelik M, Chung SA, Ardalan K, et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Kawasaki Disease. Arthritis Rheumatol. 2022;74(4):586-596. doi:10.1002/art.42041
- 2019 European recommendations: de Graeff N, Groot N, Ozen S, et al. European consensus-based recommendations for the diagnosis and treatment of Kawasaki disease – the SHARE initiative. Rheumatology (Oxford). 2019;58(4):672-682. doi:10.1093/rheumatology/key344
- 2020 Japanese guidelines: Fukazawa R, Kobayashi J, Ayusawa M, et al. JCS/JSCS 2020 Guideline on Diagnosis and Management of Cardiovascular Sequelae in Kawasaki Disease. Circ J. 2020;84(8):1348-1407. doi:10.1253/circj.CJ-19-1094
This episode focused on Kawasaki disease (KD)! Let’s start with the definition and clinical manifestations
- KD is a vasculitis of medium-sized arteries
- The disease was first described in 1967 by Dr. Tomisaku Kawasaki in a landmark paper entitled “Acute Febrile Mucocutaneous Syndrome With Lymphoid Involvement With Specific Desquamation of the Fingers and Toes in Children” in the Japanese journal Arerugi (“Allergy”). This is now known universally as Kawasaki disease, although he did not use that term himself.
- Read more about Dr. Tomisaku Kawasaki in this PIDJ In Memoriam: Shulman ST, Takahashi M. In Memoriam: Dr Tomisaku Kawasaki. J Pediatric Infect Dis Soc. Published online July 24, 2020. doi:10.1093/jpids/piaa081
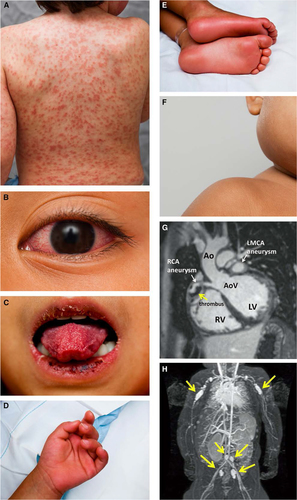
- The diagnosis of KD is made with the following definition: Fever for ≥5 days in addition to the presence of 4 of the following 5 clinical criteria:
- Bilateral injection of bulbar conjunctivae with limbic sparing and without exudate
- Erythematous mouth and pharynx, strawberry tongue, and red, cracked lips
- A polymorphous, generalized, erythematous rash, often with accentuation in the groin (which can be morbilliform, maculopapular, scarlatiniform, or erythema multiforme-like)
- Changes in the peripheral extremities consisting of erythema of the palms and soles and firm, sometimes painful, induration of the hands and feet, often with periungual desquamation usually beginning 10-14d after fever onset
- Acute nonsuppurative (usually unilateral) anterior cervical lymphadenopathy with at least 1 node ≥1.5 cm in diameter
- Madan discussed how remembering that this is a vasculitis can assist you in understanding what physical changes might manifest (rather than just memorizing the clinical criteria)! The clinical features reflect inflammation of medium-sized muscular arteries
- KD should be considered even before that 5th day of fever if several of the primary clinical criteria are present without an alternative explanation
- The clinical manifestations may appear and self-resolve at different times (rather than all being present simultaneously) → make sure to ask about prior presence of relevant manifestations when you see a child for persistent fever
- KD diagnosis is sometimes delayed, especially when fever and unilateral neck swelling is thought to be bacterial lymphadenitis or para- or retropharyngeal infection (a useful distinguishing feature would be that suppuration generally is NOT observed in KD)
- Another common consideration in the post-COVID era is the possibility of MIS-C vs KD (remember that children with MIS-C often have a wider spectrum of symptoms, are typically older, and show greater elevation of inflammatory markers)
- Coronary artery abnormalities are serious sequelae of Kawasaki disease, occurring in 20% to 25% of untreated children. If coronary artery aneurysm or ectasia is evident (z score ≥2.5) in any patient evaluated for fever, a presumptive diagnosis of KD should be made
- A normal early echo is typical and does not exclude the diagnosis but may be useful in evaluation of patients with suspected incomplete Kawasaki disease
- In one study, 80% of patients with Kawasaki disease who ultimately developed coronary artery disease had abnormalities (z score ≥2.5) on an echocardiogram obtained during the first 10 days of illness.
- Increased risk of developing coronary artery abnormalities is associated with male sex; age <12 months or >8 years; fever for more than 10 days; white blood cell count >15 000/mm3; high relative neutrophil (>80%) and band count; low hemoglobin concentration (<10 g/dL); hypoalbuminemia, hyponatremia, or thrombocytopenia; and fever persisting or recurring >36 hours after completion of Immune Globulin Intravenous (IGIV) administration.
- Aneurysms of the coronary arteries most typically occur between 1 and 4 weeks after onset of illness; onset later than 6 weeks is extremely uncommon
- In children with only mild coronary artery dilation, coronary artery dimensions often return to baseline within 6-8 wks after onset of disease
- **Irritability**, abdominal pain, diarrhea, vomiting
- urethritis with sterile pyuria (70% of cases)
- mild anterior uveitis (80%)
- mild elevation of serum hepatic aminotransferase concentrations (50%)
- arthralgia or arthritis (10%–20%)
- marked irritability with cerebrospinal fluid pleocytosis (40%)
- hydrops of the gallbladder (<10%)
- pericardial effusion of at least 1 mm (<5%)
- myocarditis manifesting as congestive heart failure (<5%)
- cranial nerve palsy (<1%)
- Persistent resting tachycardia and a hyperdynamic precordium are common findings, and an S3 gallop can be present.
- Fine desquamation in the groin area can occur in the acute phase of disease (Fink sign)
- Bullous, vesicular, or petechial rashes
- Oral ulcers
- Pharyngeal or conjunctival exudates
- Generalized lymphadenopathy
- Splenomegaly
- Leukopenia or relative lymphocyte predominance
- Other notes on clinical features and diagnosis:
- Madan and Jack discussed concurrent viral upper respiratory infections, which are sometimes present in patients with KD, should not delay diagnosis and treatment of KD
- One possible exception is that in a patient with fever, exudative conjunctivitis, and exudative pharyngitis with +Adenovirus, it’s like that the syndrome represents Adenovirus (and that KD is unlikely)
- There is no specific diagnostic test for KD. Madan also discussed how you need to consider the clinical criteria in context of your patient → sometimes this might mean not following strict criteria and considering the diagnosis still in children that might look pathophysiologically like they have KD (that may benefit from treatment). See more on incomplete KD below too
- Madan and Jack discussed concurrent viral upper respiratory infections, which are sometimes present in patients with KD, should not delay diagnosis and treatment of KD
What about incomplete Kawasaki disease? Sometimes previously called “atypical” KD
- The diagnosis of incomplete KD should be considered in children with unexplained fever who lack the clinical criteria noted above
- In these cases, supportive lab and echo data are obtained when considering the diagnosis
- A high index of suspicion must be maintained for infants (especially under 6 months of age) who have a higher risk of incomplete manifestations, delayed diagnosis, and development of coronary artery aneurysms
- Consider KD in infants under 1 year old with prolonged unexplained fever, with or without aseptic meningitis, with evidence of systemic inflammation (even with fewer than 2 of the characteristic features of KD)
- KD can also present with shock-like syndrome in infants and children without evidence an inciting infection and in those with presumed bacterial cervical lymphadenitis or para- or retropharyngeal phlegmon that fail to respond to appropriate antibiotic therapy
- Check out Fig 3.12 in AAP Red Book (2021-2024 report at the time of these Consult Notes) for flowchart on evaluation of suspected incomplete Kawasaki disease
- That chart is also available in 2017 AHA guidance for Kawasaki disease (Figure 3): McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association [published correction appears in Circulation. 2019 Jul 30;140(5):e181-e184]. Circulation. 2017;135(17):e927-e999. doi:10.1161/CIR.0000000000000484
Considering epidemiology of Kawasaki disease
- Peak age of occurrence in the US is 6-24 months
- 50% of patients are younger than 2 years old
- 80% are younger than 5 years
- Cases are uncommon in children older than 8 yo but rare cases have occurred even in adults
- The incidence of KD is greatest in children who live in East Asia or are of Asian ancestry
- In Japan, KD is a reportable disease with a incidence of almost 1 in every 100 Japanese children developing KD by age 5: Nakamura Y, Yashiro M, Uehara R, et al. Epidemiologic features of Kawasaki disease in Japan: results of the 2007-2008 nationwide survey. J Epidemiol. 2010;20(4):302-307. doi:10.2188/jea.je20090180
- In the US, there has been an estimated overall annual incidence of 20 per 100k children under the age of 5 with highest annual incidence among Asian and Pacific Islander populations (although US only has passive surveillance): Holman RC, Belay ED, Christensen KY, Folkema AM, Steiner CA, Schonberger LB. Hospitalizations for Kawasaki syndrome among children in the United States, 1997-2007. Pediatr Infect Dis J. 2010;29(6):483-488. doi:10.1097/INF.0b013e3181cf8705
- Current case-fatality rate for KD in the US and Japan is <0.2%
- Principle cause of death is myocardial infarction resulting from coronary artery occlusion attributable to thrombosis of progressive stenosis
- The relative risk of mortality is highest within 6 weeks of onset of acute symptoms, but myocardial infarction and sudden death can occur months to years after the acute episode.
- The prevalence of coronary artery abnormalities is higher if treatment (Immune Globulin Intravenous) is delayed beyond the 10th day of illness.
What causes Kawasaki disease?
- Etiology is unknown, but epidemiologic and clinical features suggest an infectious and/or environmental cause or trigger in genetically susceptible individuals. The incubation period is unknown
- As Madan discussed, reports demonstrated declines in many respiratory viral infections with pandemic mitigation efforts along with noted declines in KD (a few references on that below) → which would align with the leading theory that KD is triggered by a ubiquitous infectious agent
- Shulman ST, Rowley AH. An Unintended Consequence of Pandemic Control Measures: Fewer Cases of Kawasaki Disease. J Pediatr. 2021;239:11-14. doi:10.1016/j.jpeds.2021.08.069
- Shulman S, Geevarghese B, Kim KY, Rowley A. The Impact of Social Distancing for COVID-19 Upon Diagnosis of Kawasaki Disease. J Pediatric Infect Dis Soc. 2021;10(6):742-744. doi:10.1093/jpids/piab013
- Phamduy TT, Smith S, Herbst KW, et al. Kawasaki Disease Hospitalizations in the United States 2016-2020: A Comparison of Before and During the Coronavirus Disease 2019 Era. Pediatr Infect Dis J. 2021;40(11):e407-e412. doi:10.1097/INF.0000000000003289
- Ae R, Shibata Y, Kosami K, Nakamura Y, Hamada H. Kawasaki Disease and Pediatric Infectious Diseases During the Coronavirus Disease 2019 Pandemic. J Pediatr. 2021;239:50-58.e2. doi:10.1016/j.jpeds.2021.07.053
- Burney JA, Roberts SC, DeHaan LL, et al. Epidemiological and Clinical Features of Kawasaki Disease During the COVID-19 Pandemic in the United States. JAMA Netw Open. 2022;5(6):e2217436. Published 2022 Jun 1. doi:10.1001/jamanetworkopen.2022.17436
- That theory has also been supported by the frequent epidemics and outbreaks of KD worldwide along with the typical winter-spring seasonality
- Important work from Dr. Anne Rowley and colleagues has showed a targeted response to a specific protein antigen in children with KD, supporting one predominant causative agent for the pathogenesis of KD
- Plasmablasts (precursors to antibody-producing plasma cells) are clonally expanded in peripheral blood of children with KD at 1-2 wks after fever onset, indicating an antigen-driven immunologic response to a recent infection. These plasmablasts encode antibodies that recognize antigen in intracytoplasmic inclusion bodies in ciliated bronchial epithelial cells of children who died of KD. Rowley AH, Baker SC, Arrollo D, et al. A Protein Epitope Targeted by the Antibody Response to Kawasaki Disease. J Infect Dis. 2020;222(1):158-168. doi:10.1093/infdis/jiaa066
- Rowley AH, Baker SC, Shulman ST, et al. Ultrastructural, immunofluorescence, and RNA evidence support the hypothesis of a “new” virus associated with Kawasaki disease. J Infect Dis. 2011;203(7):1021-1030. doi:10.1093/infdis/jiq136
- They modified the epitope sequence and found the revised epitope was recognized by monoclonal antibodies derived from plasmablasts isolated in 11/12 patients with KD and that these antibodies show convergent VH3-74 heavy chain usage, supporting idea of single predominant causative agent Rowley AH, Arrollo D, Shulman ST, et al. Analysis of Plasmablasts From Children With Kawasaki Disease Reveals Evidence of a Convergent Antibody Response to a Specific Protein Epitope. J Infect Dis. 2023;228(4):412-421. doi:10.1093/infdis/jiad048
Management of Kawasaki disease
- The goal of treatment during the acute phase is to decrease inflammation of the myocardium and coronary artery wall and provide supportive care → after the acute phase, therapy is directed at preventing coronary artery thrombosis
- Primary treatment includes a single dose of IVIG 2g/kg, administered over 10-12 hrs, and aspirin
- This typically results in rapid resolution of fever and lab changes in ~85% of patients
- IVIG given within 10d of fever onset reduces the risk of coronary artery aneurysms from 17-25% down to <5%
- IVIG is most effective if given within 7-10d of illness but still given after 10d in patients with persistent fever, ongoing signs of systemic inflammation, and/or coronary artery aneurysms
- The mechanism is not totally clear
- Aspirin is used for its anti-inflammatory and antithrombotic activity, although aspirin alone does not decrease the risk of coronary artery abnormalities. There is variability in dosing of aspirin, as discussed on the show:
- Some use 30-50 mg/kg/day (in 4 divided doses) while others use 80-100 mg/kg/day (in 4 divided doses) → There is little data to suggest which aspirin dose is superior
- The lower dose of 30-50 mg/kg/d is recommended by AHA and AAP given higher doses have increased potential for adverse effects without confirmed benefits
- Aspirin is held if there is a contraindication including infection with varicella or influenza
- Broderick C, Kobayashi S, Suto M, Ito S, Kobayashi T. Intravenous immunoglobulin for the treatment of Kawasaki disease. Cochrane Database Syst Rev. 2023;1(1):CD014884. Published 2023 Jan 25. doi:10.1002/14651858.CD014884.pub2
- Terai M, Shulman ST. Prevalence of coronary artery abnormalities in Kawasaki disease is highly dependent on gamma globulin dose but independent of salicylate dose. J Pediatr. 1997;131(6):888-893. doi:10.1016/s0022-3476(97)70038-6
- Newburger JW, Takahashi M, Beiser AS, et al. A single intravenous infusion of gamma globulin as compared with four infusions in the treatment of acute Kawasaki syndrome. N Engl J Med. 1991;324(23):1633-1639. doi:10.1056/NEJM199106063242305
- Newburger JW, Takahashi M, Burns JC, et al. The treatment of Kawasaki syndrome with intravenous gamma globulin. N Engl J Med. 1986;315(6):341-347. doi:10.1056/NEJM198608073150601
- Durongpisitkul K, Gururaj VJ, Park JM, Martin CF. The prevention of coronary artery aneurysm in Kawasaki disease: a meta-analysis on the efficacy of aspirin and immunoglobulin treatment. Pediatrics. 1995;96(6):1057-1061.
- Furusho K, Kamiya T, Nakano H, et al. High-dose intravenous gammaglobulin for Kawasaki disease. Lancet. 1984;2(8411):1055-1058. doi:10.1016/s0140-6736(84)91504-6
- Dallaire F, Fortier-Morissette Z, Blais S, et al. Aspirin Dose and Prevention of Coronary Abnormalities in Kawasaki Disease. Pediatrics. 2017;139(6):e20170098. doi:10.1542/peds.2017-0098
- Kuo HC, Lo MH, Hsieh KS, Guo MM, Huang YH. High-Dose Aspirin is Associated with Anemia and Does Not Confer Benefit to Disease Outcomes in Kawasaki Disease. PLoS One. 2015;10(12):e0144603. Published 2015 Dec 10. doi:10.1371/journal.pone.0144603
- Dhanrajani A, Chan M, Pau S, Ellsworth J, Petty R, Guzman J. Aspirin Dose in Kawasaki Disease: The Ongoing Battle. Arthritis Care Res (Hoboken). 2018;70(10):1536-1540. doi:10.1002/acr.23504
- Adjunctive therapies include:
- In high-risk / severe cases, could consider addition of corticosteroids. Steroids used to be a hallmark but later found to be ineffective or potentially harmful → now reserved for use in conjunction with IVIG
- TNF-alpha agents such as etanercept or infliximab have been studied as adjuvant therapy
- Some articles:
- Dionne A, Burns JC, Dahdah N, et al. Treatment Intensification in Patients With Kawasaki Disease and Coronary Aneurysm at Diagnosis. Pediatrics. 2019;143(6):e20183341. doi:10.1542/peds.2018-3341
- Choueiter NF, Olson AK, Shen DD, Portman MA. Prospective open-label trial of etanercept as adjunctive therapy for kawasaki disease. J Pediatr. 2010;157(6):960-966.e1. doi:10.1016/j.jpeds.2010.06.014
- Tremoulet AH, Jain S, Jaggi P, et al. Infliximab for intensification of primary therapy for Kawasaki disease: a phase 3 randomised, double-blind, placebo-controlled trial. Lancet. 2014;383(9930):1731-1738. doi:10.1016/S0140-6736(13)62298-9
- Portman MA, Dahdah NS, Slee A, et al. Etanercept With IVIg for Acute Kawasaki Disease: A Randomized Controlled Trial. Pediatrics. 2019;143(6):e20183675. doi:10.1542/peds.2018-3675
- Some articles:
A few additional follow-up considerations
- Echocardiography should be performed at the time of suspected diagnosis and repeated at 2 weeks and 6 to 8 weeks after diagnosis in children with normal coronary arteries on initial evaluation.
- Long-term management and cardiac care of a child with KD will be based on extent of coronary artery involvement (which will be coordinated with your friendly neighborhood pediatric cardiologist!)
- Development of giant coronary artery aneurysms (luminal diameter ≥8 mm or larger in a child, but smaller diameter in an infant based on relative body surface area, z score ≥10) usually requires addition of anticoagulant therapy, such as warfarin or low-molecular weight heparin, to prevent thrombosis.
- The average duration of fever in untreated Kawasaki disease is 10 days; however, fever can last 2 weeks or longer.
- After fever resolves, patients can remain anorexic and/or irritable with decreased energy for 2 to 3 weeks.
- During this phase, desquamation of fingers, toes, hands, and feet may occur. Transverse lines across the nails (Beau’s lines) sometimes are noted month(s) later.
- Recurrent disease develops in approximately 1-2% of children in the US at a median of 1.5 years after index episode
- Reminder/Pearl: Measles- and varicella-containing vaccines (MMRV) should be deferred until 11 months after receipt of IGIV, 2 g/kg, for treatment of Kawasaki disease because of possible interference with development of an adequate immune response
A few other references
- Some surveillance studies (older now):
- Morens DM, Anderson LJ, Hurwitz ES. National surveillance of Kawasaki disease. Pediatrics. 1980;65(1):21-25.
- Burns JC, Mason WH, Glode MP, et al. Clinical and epidemiologic characteristics of patients referred for evaluation of possible Kawasaki disease. United States Multicenter Kawasaki Disease Study Group. J Pediatr. 1991;118(5):680-686. doi:10.1016/s0022-3476(05)80026-5
Infographics
Goal
Listeners will be able to explain the clinical presentation, diagnosis, and management of Kawasaki disease
Learning Objectives
After listening to this episode, listeners will be able to:
- Recognize the clinical presentation of KD along with other diseases that may be on the differential
- Discuss the use of diagnostic clinical criteria for KD and incomplete KD
- Identify the importance of prompt IVIG administration in KD, which can prevent coronary aneurysms
Disclosures
Our guests as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Flores, J., Kumar, M., Dong, S. “#96: Riddle Me This”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/5058f3c5-8b3b-4757-8413-b0798cde32b8