Table of Contents
Credits
Hosts: Zach Lorenz, Sara Dong
Guests: Morgan Walker, Olivia Kates
Writing: Zach Lorenz, Morgan Walker, Sara Dong
Producing/Editing/Cover Art: Sara Dong
Infographics: Zach Lorenz, Sara Dong
Our Guests
Guest Co-Host
Zach Lorenz, MD
Dr. Zach Lorenz is a PGY-3 Internal Medicine resident physician at Johns Hopkins Bayview Medical Center. Check out his prior episode as well, #21 Sailor’s Salutation, for an excellent discussion on syphilis
Guest Discussant
Morgan Walker, MD

Dr. Morgan Walker is an Infectious Diseases & Critical Care Medicine fellow at Johns Hopkins Hospital and NIH.
Guest Discussant
Olivia Kates, MD

Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Culture
Olivia: Prey, 2022 action/sci-fi film, available on Hulu
Morgan: her new Bulldog puppy, Magnolia!
Zach: Dune, by Frank Herbert, 1965 scifi novel
Consult Notes
Consult Q
“Team is concerned for Mucor. Should we start Amphotericin?”
Case Summary
29 year old woman with Type 1 Diabetes Mellitus who was found to have invasive fungal rhinosinusitis
Key Points
Message from the primary author, Zach: This episode is dedicated to the memory of our patient, who served as the inspiration for this episode (although certain features have been de-identified), and taught me a lot about this diagnosis.
The term fungal rhinosinusitis includes a wide variety of fungal infections, but these consult notes and the episode will focus on acute invasive fungal rhinosinusitis
- *Although this diagnosis can occur in immunocompetent patients, the majority of cases will involve patients with some form of immunosuppression or immunocompromising condition* Some of the common underlying diseases include:
- Hematologic malignancy
- Hematopoietic cell transplantation
- Chemotherapy-induced neutropenia
- Solid organ transplant
- Advanced HIV
- Diabetes mellitus
- Glucocorticoids (systemic or intranasal)
- Has a time course of days to a few weeks
- Involves hyphal invasion of blood vessels with resulting tissue infarction
- Infection may be attributable to invasion by fungi that chronically colonize the sinuses or inhalation of fungal spores
- The degree of tissue invasion and how aggressive the disease will be varies by the underlying immune status of the host
- The spread of infection outside of the sinuses is usually due to direct extension, but fungemia with metastatic spread is possible
- Some resources:
- deShazo RD, Chapin K, Swain RE. Fungal sinusitis. N Engl J Med. 1997;337(4):254-259. doi:10.1056/NEJM199707243370407
- Chakrabarti A, Denning DW, Ferguson BJ, et al. Fungal rhinosinusitis: a categorization and definitional schema addressing current controversies. Laryngoscope. 2009;119(9):1809-1818. doi:10.1002/lary.20520
- Roden MM, Zaoutis TE, Buchanan WL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41(5):634-653. doi:10.1086/432579
Microbiology of acute invasive fungal rhinosinusitis
- Acute fulminant infections are usually related to Aspergillus, Fusarium, or Mucorales
- Other fungi, such as dematiaceous molds or other hyaline molds, can also cause disease > sometimes in a more indolent/chronic manner
- Candida species typically are not the culprit despite their ability to colonize the sinuses, although there are case reports of invasive rhinosinusitis with Candida
Clinical presentation & Initial Evaluation
- Diagnostic clues that suggest invasive fungal rhinosinusitis in an immunocompromised patient include:
- Fever, epistaxis, facial pain, nasal congestion, headache
- Changes in vision or mentation
- Facial numbness or diplopia with cranial nerve involvement
- Proptosis and fixation of globe can be seen with orbital involvement
- There MUST be a high degree of suspicion in immunocompromised patients with new sinus complaints and/or facial pain!!
- Imaging (CT or MRI) can show sinus involvement and may reveal bony extension of the infection to the globe, brain, cavernous sinus, or carotid artery
- CT: higher sensitivity for bony erosion
- Vs
- MRI: higher sensitivity for soft tissue abnormalities (such as intracranial, intraorbital, cavernous sinus involvement)
- It is critical to have early endoscopic evaluation by an otolaryngologist!
- Nares and oral cavity should be examined for necrotic areas
- Necrosis from vascular invasion can appear as palatal or gingival eschars or as sloughing of nasal septum (and may progress to perforation of nasal septum)
- Some resources:
- Aribandi M, McCoy VA, Bazan C 3rd. Imaging features of invasive and noninvasive fungal sinusitis: a review. Radiographics. 2007;27(5):1283-1296. doi:10.1148/rg.275065189
- Roithmann R, Shankar L, Hawke M, Chapnik J, Kassel E, Noyek A. Diagnostic imaging of fungal sinusitis: eleven new cases and literature review. Rhinology. 1995;33(2):104-110.
Diagnosis of invasive fungal rhinosinusitis
- Evaluation of patients with suspected fungal rhinosinusitis should include early nasal endoscopy with biopsies of affected tissues (as mentioned above)
- Tissue biopsies should be obtained from the eschar as well as viable areas abutting the necrotic tissue
- These biopsies assist in detecting vascular invasion and examining the morphology of the fungus >> as well as being sent for culture
- Generally patients are also undergoing debridement of necrotic tissue as able in the same setting
- Definitive diagnosis depends on histopathologic demonstration of fungal invasion by biopsy, and isolation of the infecting fungus is important to guide therapy
- CT/MRI imaging is not sensitive/specific enough to confirm the diagnosis, but this is helpful to define the extent of disease
Fungal morphology in tissue (with some throwback graphics)
- In tissue, Mucorales hyphae can often be distinguished from other more common opportunistic molds (like Aspergillus and Fusarium) by their broad, empty, thin-walled, and mostly aseptate hyphae
- Frequently these hyphae have focal bulbous dilation and non dichotomous irregular branching at occasional right angles (90 degrees)
- Reproductive hyphal structures containing spores are rarely observed in deep tissue
- Check out this prior infographic as a review:
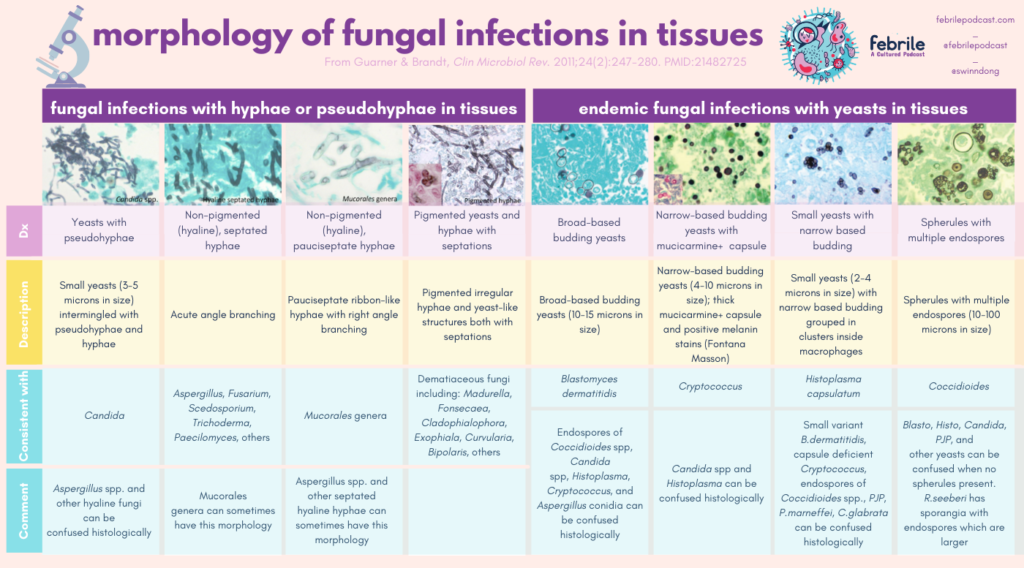
- Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24(2):247-280. doi:10.1128/CMR.00053-10
- As mentioned on the episode, if the micro/path team knows that you are considering mucorales, the focus on sample preparation may be more “mincing” rather than grinding
- Grinding mucorales in tissue will produce small fragments devoid of any enclosing septal cell walls (the septations kind of house the different nucleic and cytoplasm for the fungus to grow) >> so mincing or handling the sample differently may help avoid disrupting the tissue enough to the point where you aren’t able to culture it
- You can also refer this infographic for fungal markers
Treatment of invasive rhinosinusitis
- Management of this infection is challenging as it is difficult to cure and most affected patients are immunocompromised
- Overall survival can be poor, and survivors often have significant complications (especially if intracranial involvement)
- Initial empiric therapy should be started asap for those with signs and symptoms and risk factors with Amphotericin B
- As discussed on the episode, you would start a minimum of 5 mg/kg – although some would push towards 10 mg/kg/day if patient could tolerate
- Another key factor in treatment is immune status:
- Can any immunosuppressive medications be withdrawn?
- Attempting control of the underlying illness (such as with control of hyperglycemia and reversal of ketoacidosis in diabetes)
- Duration of IV therapy upfront depends on the immune status of the host, extent of surgical debridement, and response to therapy
- Many experts would continue until there is a clear clinical response as well as reversal of immunocompromising conditions (such as resolution of neutropenia, tapering of steroids, engraftment in HSCT)
- This will generally mean weeks of therapy with IV, and may require even longer if severe immunosuppression and slow clinical response
- A few additional notes:
- Morgan and Olivia touched on addition of azole, which some experts may do fairly early in the course along with the Ambisome
- Scedosporium spp are generally amphotericin B resistant >> treat with voriconazole
- Regimen of choice for Aspergillus is voriconazole, although isavuconazole is an alternative if voriconazole cannot be used
- Echinocandins (caspofungin, micafungin, anidulafungin) can be added for patients with severe disease
- Surgical debridement is a cornerstone of management
- Sinus surgery is an independent prognostic factor for survival
- The goal of primary endoscopic surgery = resection of involved mucosa and bone (such as endoscopic medial maxillectomy, septectomy, and more)
- Intraoperative frozen sections often guide the extent of debridement
- The impact on survival is attributed to decreased fungal burden and removal of avascular necrotic tissue (which antifungals have trouble penetrating)
- This also facilitates postoperative endoscopic monitoring for remaining disease
- The goal of primary endoscopic surgery = resection of involved mucosa and bone (such as endoscopic medial maxillectomy, septectomy, and more)
- Many consider this diagnosis a surgical emergency, although there has only been limited investigation into the optimal timing of surgery
- One study found that surgical delay >6 days was associated with decreased survival:
- But this noted no difference when surgery was performed between days 1-30:
- Extension of fungal involvement into the orbit significantly increases mortality and poses surgical challenges
- Extending debridement to include orbital exenteration has not been shown to improve survival in studies, but it’s unclear whether this is just a reflection of more aggressive underlying disease – but it does raise uncertainty into the potential benefits of exenteration vs morbidity and disfigurement
- Orbital exenteration is a decision made on a case by case basis
- Intracranial extension also has a poor prognosis and the role of craniotomy must be carefully weighed
- Sinus surgery is an independent prognostic factor for survival
- Ultimately patients can be transitioned to oral antifungal therapy, typically posaconazole or isavuconazole in the setting of mucormycosis or voriconazole with Aspergillus
- Duration of suppressive therapy is usually at least 3-6 months, but certain patients will remain on lifelong therapy – ultimately this decision is made on a case by case basis as well
- Resources:
- Valera FC, do Lago T, Tamashiro E, Yassuda CC, Silveira F, Anselmo-Lima WT. Prognosis of acute invasive fungal rhinosinusitis related to underlying disease. Int J Infect Dis. 2011;15(12):e841-e844. doi:10.1016/j.ijid.2011.08.005
- Turner JH, Soudry E, Nayak JV, Hwang PH. Survival outcomes in acute invasive fungal sinusitis: a systematic review and quantitative synthesis of published evidence. Laryngoscope. 2013;123(5):1112-1118. doi:10.1002/lary.23912
- Weber R, Draf W, Kratzsch B, Hosemann W, Schaefer SD. Modern concepts of frontal sinus surgery. Laryngoscope. 2001;111(1):137-146. doi:10.1097/00005537-200101000-00024
- Roxbury CR, Smith DF, Higgins TS, et al. Complete surgical resection and short-term survival in acute invasive fungal rhinosinusitis. Am J Rhinol Allergy. 2017;31(2):109-116. doi:10.2500/ajra.2017.31.4420
- Hargrove RN, Wesley RE, Klippenstein KA, Fleming JC, Haik BG. Indications for orbital exenteration in mucormycosis. Ophthalmic Plast Reconstr Surg. 2006;22(4):286-291. doi:10.1097/01.iop.0000225418.50441.ee
- Trief D, Gray ST, Jakobiec FA, et al. Invasive fungal disease of the sinus and orbit: a comparison between mucormycosis and Aspergillus. Br J Ophthalmol. 2016;100(2):184-188. doi:10.1136/bjophthalmol-2015-306945
- Monroe MM, McLean M, Sautter N, et al. Invasive fungal rhinosinusitis: a 15-year experience with 29 patients. Laryngoscope. 2013;123(7):1583-1587. doi:10.1002/lary.23978
- Marty FM, Ostrosky-Zeichner L, Cornely OA, et al. Isavuconazole treatment for mucormycosis: a single-arm open-label trial and case-control analysis. Lancet Infect Dis. 2016;16(7):828-837. doi:10.1016/S1473-3099(16)00071-2
- Melancon CC, Clinger JD. The Use of Frozen Section in the Early Diagnosis of Acute Invasive Fungal Sinusitis. Otolaryngol Head Neck Surg. 2017;157(2):314-319. doi:10.1177/0194599817697279
- Munir N, Jones NS. Rhinocerebral mucormycosis with orbital and intracranial extension: a case report and review of optimum management. J Laryngol Otol. 2007;121(2):192-195. doi:10.1017/S0022215106003409
Infographics
Goal
Listeners will be able to diagnose and manage acute invasive fungal rhinosinusitis
Learning Objectives
After listening to this episode, listeners will be able to:
- Describe the typical clinical presentation of acute invasive fungal sinusitis in an immunocompromised host
- Compare and contrast histopathology of Mucorales in tissue compared to other common fungal infections
- Discuss the importance of multidisciplinary management of invasive fungal rhinosinusitis, including antifungal therapy as well as surgical evaluation
Disclosures
Our guests (Zach Lorenz, Morgan Walker, Olivia Kates) as well as Febrile podcast and hosts report no relevant financial disclosures
Citation
Walker, M., Kates, O., Lorenz, Z., Dong, S. “#66: All the Right Angles”. Febrile: A Cultured Podcast. https://player.captivate.fm/episode/5235d18d-f57f-45e3-bc54-c4ffaebbcc56